The dental implants have been successful, which has prompted study into methods to reduce surgical complexity and improve survival. Even in the most critical case, the use of implants has expanded as a result of advanced technology. Reduced bone height and volume as a result of bone resorption after tooth extraction renders implant placement difficult. In situations when the standard implants are not feasible, shorter implants have been proposed as an alternative. It's uncertain if they offer an effective course of treatment. Short implants shorten the duration of treatment, simplify the implant procedure, reduce patient morbidity, and reduce treatment costs. Despite the advantages they provide, a range of biological consequences that may even result in their elimination have been documented in the literature. This review focuses on the biomechanical considerations, the factors that affects the success of the short implants and their feasibility to be used as a viable therapeutic option for the rehabilitation of atrophic maxillary and mandibular alveolar ridges.
Introduction
Bone resorption following tooth extraction result in reduced bone height and volume can be limitation to place implant [1]. Following tooth extraction, the posterior region of the maxilla and the mandible show differing patterns of bone loss. Maxilla has slower vertical loss and a larger horizontal loss in the buccal-palatal direction. The natural height remodelling of the bone and maxillary sinus pneumatization cause the maxilla's vertical bone loss in two different directions. The mandibular vertical bone loss, on the other hand, primarily affects the vertical direction and typically results in a decreased bone height but with reasonable amount of bone at the horizontal plane. The planning of atrophic arches’ posterior sites is normally more complex because of this type of bone loss and presence of vital anatomical structure. Due to the expansion of the maxillary sinus following tooth loss and the mandibular canal being 10 mm or more above the inferior border of the mandibular body, the posterior parts of the jaws typically have the least amount of bone height [2]. Several techniques such as guided bone regeneration (GBR), block grafts sinus augmentation, and distraction osteogenesis has been proposed to increase the deficient residual ridge height prior to the placement of the implant. Though they are considered to be successful, they are sensitive, highly challenging and has got increase risk involved. Therefore, use of short implant have been solutions for these cases. Implant that are less the 10mm are considered to be short implant. Simplifying the complex surgical and prosthetic need make the implant placement more acceptable and affordable [1]. Generally, the most frequent parameters that are need to be assessed are the marginal bone loss and the cumulative implant survival rate, followed by implant failure rate and biological complications such as bleeding on probing and probing pocket depth [3]. With improvement in the implant surface geometry and surface texture, there is an increase in the bone implant contact area that provides a good primary stability during osseo-integration. Six short implants are used to support a fixed prosthesis, or four short implants are used to support an overdenture in the treatment of a severely resorbed edentulous mandible. Two additional short-length implants are placed in the distal region of the edentulous maxilla, in addition to longer implants in the premaxilla, to support a fixed prosthesis or maxillary overdenture [4]. The aim of this article is to familiarize the reader with use of short implant under different clinical scenarios.
History
In 1968, Thomas Driskell developed the Bicon dental implant system (Figure 1), launching the 8-mm implant. The shortest conventional endosseous implants that could be found were 10 mm long until 1979. Braunemark introduced the 7-mm implant this year. As the result of this, implants be divided into short implants and ultra short implants. Implants that are termed conventional “short implants” ranging from 7 mm to 10mm length and “ultrashort implants” of length <7 mm. The Bicon system had also introduced a 5-mm height implant and received the Food and Drug Administration (FDA) approval in 2008 [5].
Bicom system is completely different from other system. Dr Vincent J. Morgan, Founder and President of the company, made it very special. They believe there is no logic behind threaded implants and high speed drilling. Bicom system has got only three threads. The pressure and heat lead to the degeneration of bone. They obliterate bone. When Driskell first began employing slow drilling in 1968, he was aware of this phenomenon. There are several benefits of slow drilling. Our patient will be more comfortable, we can harvest the bone, we have excellent sight, we won't run the danger of bone necrosis.
|
|
|
Figure 1. Bicon implant sytem |
Because the bone surrounding the short implant is Haversian and cortical in nature, with better mechanical qualities than the appositional bone surrounding threaded implants, the short implant functions effectively. An implant's macro-geometry holds the key to its capabilities. Bicon’s osteotomy is prepared with slow drilling of about 50 RPM, or even slower with hand reamers. When the implant is inserted into the osteotomy, blood develops in its plateaus and immediately transforms into Haversian bone that resembles cortex in the absence of osteoclastic activity. On the other hand, pressure is applied to the bone when a threaded implant is screwed into it [6].
Although primary stability is a topic of discussion, osteoclastic activity is the first thing that occurs when an implant is screwed into bone. The bone grows back towards the threaded implant as appositional bone, or bone without blood vessels. The mechanical characteristics of this appositional bone are completely different from those of the Haversian bone surrounding implants, which may account for the greater success rate of short implants [7].
Over a period of more than thirty years, Thomas Driskell's Bicon dental implant design has proven to be effective due to the prosthetic restorations performed on this model [8].
Biomechanical consideration
Diagnostic
Implant diameter
The area receiving the most Stress is the bone crest, and relatively little stress is passed to the apical section.A longer implant would only enhance primary stability whereas, a wider implant would enhance primary stability as well as the functional surface area at the crustal bone level, improving the distribution of occlusal stresses. A finite element analysis by Himmlová et al. reported that a larger implant diameter reduced stress around the implant neck and more effectively dispersed the simulated masticatory force [9] Gavali et al. also in parallel with the above author reported that Increase in implant length will increase the total surface area of the implant and improve the primary stability, this is by increasing the bone implant contact (BIC). However, the functional surface area (FSA)—that is, the region that transmits the compressive and tensile stresses to bone—is limited to the crestal 5-7 mm. Increasing the length of the implant will not alter this. nevertheless, a shorter implant with a wider diameter offers enhanced primary stability as well as greater FSA [10].
Crown/implant ratio
A molar tooth can be supported for decades by an ankylosed tooth with a minimally sized root. Also with advancements in surfaces and implant systems, together with optimal force direction and load distribution, have made it possible to successfully use high crown/implant ratios [11] Meijer et al. reviewed and reported that the crown-to-implant ratio of nonsplinted, single-tooth implants ranged from 0.86 to 2.14, indicating a low occurrence of biological or technological issues [12]. da Rocha Ferreira et al. considering other factors such as the implant’s diameter, micro and macro geometry, implant-abutment connection, bone’s quality and volume, surgical protocols or the passive fit of the prosthetic components concluded that the primary cause of the marginal bone stress generation is due to high crown height space. There appears to be a potential paradigm shift in which the prosthetic height takes precedence over the length of the implants or the proportion between the height of the prosthesis and the length of the implants. Under these circumstances, further study on this subject is required in order to create novel prosthetic designs that may lessen the stress produced at the marginal bone level [13] (Figure 2).
|
|
|
Figure 2. Crown-implant ratio |
Bone quality
Jaw bone and bone quality are the key element in the success of short implants [14]. Short implants had a 99% success rate in mandibles which predominately have type I and II bone type and a 92% success rate in maxillae which predominately have type III and type IV, according to Malo et al. the maxilla's porous bone likely affected the proportion of success attained as well as the losses [15]. Galvao et al. reviewed and reported that regardless of the surface treatment used to the implant, areas of type III and type IV bone exhibit greater failures. Insufficient bone density and a short implant length impair the stability of the implant both during implantation and the healing process [16]. Liu et al. concluded in a mandible with inferior bone quality, the bone around short implants was very susceptible to resorption [17]. Tawil, in his patient series, reported that bone quality rather than quantity seems to be the determining factor in implant longevity (Table 1) [18].
Table 1. Bone density classification by Misch [19]
|
BONE |
|
DENSITY |
|
D1 |
>1250 HU |
Dense cortical bone |
|
D2 |
850-1250 HU |
Thick dense to porous cortical bone on crest and coarse trabecular bone |
|
D3 |
350-850 HU |
Thin porous cortical bone on crest and fine trabecular bone within |
|
D4 |
150-350 HU |
Fine trabecular bone |
|
D5 |
<150 HU |
Immature, non- mineralised bone |
Lack of cantilevers
A cantilever amplifies the forces directly proportional to the height of the crown. Six alternative possible rotation points are created on the implant body. Eliminating cantilevers improves treatment predictability and promotes biomechanics [4]. Thoma et al. reported that When compared to two adjacent short implants, cantilever short implants have comparable clinical and radiological results after five years. However, they tend to fail at earlier time,suggesting an overload of the implants. Either treatment options can be indicated depending on the clinical evaluation [20].
Number of implants
Placing numerous implants will enhance the surface area that can withstand occlusal stresses [4].
Implant design
Threaded feature in implant body designs can convert occlusal loads into more favourable compressive loads at bone interface. Implant threads are developed to minimise micro movement that might jeopardise osseointegration, maximise initial contact, offer primary stability, increase surface area, causes compression of bone, and enable load dissipation at the interface between the implant and bone [21]. Bolind et al. reported that the bone implant contact was greater with the threaded implant and more marginal bone loss was seen in cylinder implants [22].
Implant body designs with threaded features have the ability to convert occlusal loads into more favorable compressive loads at the bone interface.
The implant surface area can be increased by
Thread number [4]
the implant surface area in contact with the bone increases with the increase in the number of thread per unit length in the same axial plane
Thread depth [4]
Deeper threads offer a larger implant surface area.
Thread shape (Figure 3)
Compared to v-shape and reverse buttress thread designs, the square thread design has a larger percentage of bone-implant contact [4]. Ten times more shear force occurs in a V-thread and reverse buttress thread than on a square thread. The reduction in shear loading at the thread bone interface provides for more compressive load transfer, which is particularly important in poor bone density, short implant lengths, or higher force magnitude [23].
Implant surface [4]
Implant surface treatment are key factors for success with short implants. Rough micro topography of the implant surface, as opposed to a turned, smooth surface, enhances the bone-implant contact surface area and speeds osseointegration. Additionally, it makes up for a poor crown-to-implant ratio.
|
|
|
|
|
a) |
b) |
c) |
|
Figure 3. a)V Thread, b) Reverse Thread, c) Square Thread |
||
Surgical
Two step surgical protocol
For short implants, a two-stage procedure is advised because it offers high primary stability during the healing phase. Galvao et al. reviewed and reported that two stage should be performed while installing short implants and for the maxilla and the mandible, the interval between the surgical and load stages should be 4-6 months and 2-4 months, respectively [16].
Adapted surgical protocol
By eliminating a step in the standard surgical procedure, such as skipping the countersink drill or the final drill in the standard drilling sequence, one might increase the initial implant stability. While the final bone drilling should be carried out using narrow drills rather than standard drills, soft bone drilling technique should be followed in poor quality bone [24].
Prosthetic
Implant to abutment connection (Figure 4)
Castro et al. in his study concluded that when compared to external hex abutment connections, the Morse taper connection causes reduced marginal bone loss and encourages bone development across the implant shoulder [25].
Maeda et al. compared stress distribution patterns between implants with external-hex or internal-hex connection systems using in vitro models. Under horizontal load, fixtures with an exterior hex showed increased strain at the cervical area, whereas internal hex fixtures showed strain at the fixture tip area. Compared to an external hex connection, the internal hex implant abutment connection exhibits a larger force distribution [26].
|
|
|
|
|
a) |
b) |
c) |
|
Figure 4. a) External Hex, b) Morse Taper, c) Internal Hex |
||
Platform switching [4]
Maintains the crestal bone for the entire length of the implant up to the collar level [27-31].
Occlusal table [4]
A small occlusal table lowers the implant's offset loads.
Incisal guidance [4]
Implants should follow a biomechanical approach similar to natural teeth to accommodate the higher bite forces in the posterior regions of the mouth. Incisal guidance of the anterior teeth eliminates lateral forces to the posterior teeth in all mandibular excursions [32-34].
Splinting
When placing implants in soft bone, splinting them enhances the functional surface area of support and transmits less force to the prosthesis, cement, abutment screws, and the implant bone interface [4]. Ahumada-DeGirolamo et al. reviewed and concluded that implant size and how it relates to coronary height may be significant when making decisions. Additionally, for implants less than 8 mm or with an unfavourable crown-to-implant ratio, splinting adjacent crowns offers biological and biomechanical advantages. Also each clinical situation is unique and other factors like patient factor and parafunctions should be considered [35].
Factors influencing the survival rate of short implants
Any factor that raises the likelihood or potential for failure is a risk factor. There are numerous factors that have been reported in the literature that influence the use and diagnosis of short implants. In general,the quantity and quality of bone, the patient's age, the dentist's experience, the placement site, the length of the implant, axial stress, and oral hygiene care are the main indicators of implant success. Poor bone quality, chronic periodontitis, systemic diseases, smoking, untreated cavities or infections, advanced age, implant location, short implants, acentric loading, an insufficient number of implants, parafunctional habits, and lack of/loss of implant integration with hard and soft tissues are the primary predictors of implant failure. Implant failure may also be attributed to improper prosthesis design [36].
Smoking
Smoking appears to have greater negative effects on cancellous bone than it does on cortical bone, according to a rat research. In a prospective study on implant surgery, Bain reported a smoking cessation programme in which patients gave up cigarettes one week prior to and eight weeks following the procedure [37]. Smokers who adhered to this protocol had noticeably reduced implant failure rates (11.8%) compared to those who did not (38.5%). Smokers have somewhat greater failure rates (2.6% versus 1.9%, respectively) in compromised maxillary bone than nonsmokers [38].
Implant location
Maxillary insertion of short implants was not determined to be a risk factor for implant success, despite the fact that mandibular short implants had a greater success rate than maxillary short implants [39]. Kim et al. reported that most implant failures occur in the maxillary molarregion with poor bone quality [40]. In contrast, a study done Mezzomo et al. found a higher failure rate for single crowns supported by short implants in the mandible [41]. A fracture of the supporting bone tissue might be one reason for the increased risk of implant loss in the mandible compared to the maxilla. Though mandible is cortical and rigid, it is more prone to fracture and implant loss, eventually [42]. Monje et al. reviewed and reported no difference in terms of survival rates of short implants with regard to their anatomical location [1].
Periodontitis
According to literature, those with a history of periodontitis are more likely to experience biological problems (such as peri-implantitis and marginal bone loss) and have inferior implant success and/or survival rates than people without a history of the condition [43-45]. peri-implantitis considered to be the primary cause of short implant failure. In the research conducted by Hasanoglu Erbasar et al. [39], it was discovered that neither implant length nor diameter had a significant effect on the success of short implants. Its is the history of smoking and periodontitis had negative influence in the success of short implants. It is always safer to do proper periodontal treatment prior to implant placement for patients with periodontitis and that a strict, supportive periodontal program is strongly recommended for the long-term success of short implants [46-49].
Splinting
Implant splinting seems to be helpful, and connecting a shorter implant to an adjacent longer implant seems to increase its longevity in particular [5]. Study done by Akca et al. showed the group that is splinted (97.7%) and those without splinting (93.2%) had varying success rates [50]. While nonsplinted implants showed a greater failure rate when implanted in men and when implants shorter than 10 mm were used, the success of splinted implants was unrelated to any other variable. The failures in men may be due to greater bite forces although this was unclear from the data [5].
Loading protocol
Weerapong et al. studied and concluded that the survival rate, stability, and marginal bone loss in the immediate-loaded mandibular molar implants were not statistically different from those in the conventional method [51]. Ayna et al. observed that the clinical outcomes of the immediate loading protocols in the maxillary molar region were satisfactory. But as compared to the delayed approaches, the immediate loading group showed more bone loss and bleeding on probing. The posterior maxilla's poor bone quality or less probable causes, such as the operator's expertise or the insertion torque, might be responsible for this [52]. Cannizzaro et al. used a flapless technique and placed dental implants in the maxillary and mandibular regions. Immediate loading was done ,monitored the patients for nine years. They concluded that immediate placement of short implants could be clinically successful in the long term [53].
Short implants on mandible
The rehabilitation of total edentulous patients in the posterior region of the mandible can be complicated due to the lack of bone bioavailability caused by the presence of the lower alveolar nerve. In these circumstances, there is a need for increase the availability of bone height using technique such as lateralization of the alveolar nerve, Vertical ridge augmentation etc. These methods frequently result in complications like Graft contamination and postoperative infections [54-73].
Saenz-Ravello et al. reviewed and concluded that the use of short implants could decrease implant failure, Marginal bone loss and biological complications, and increase patient satisfaction in case of atrophic mandibular ridges when compared to regular implants after bone augmentation [74].
After reviewing the literature, Rosa et al. concluded that mandibular atrophy patients may benefit from fixed full-arch restorations supported by short implants [75].
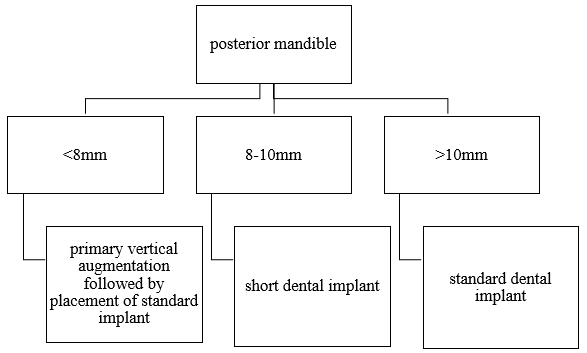
Three choices are available for the posterior mandible with a restricted alveolar ridge height: primary vertical ridge augmentation and implant installation, simultaneous implant placement with vertical ridge augmentation, and the use of short implants (Figure 5a-5c) [76].
|
|
|
|
|
a*) |
b*) |
c*) |
|
a) |
||
|
|
|
|
|
a**) |
b**) |
c**) |
|
b) |
||
|
|
|
|
|
a***) |
b***) |
c***) |
|
c) |
||
|
Figure 5. a*) A treatment option for the posterior mandible with a remaining ridge height of less than 8 mm. b*) Primary vertical bone augmentation should be performed. c*) followed by the placement of standard-length implants. a**) A treatment option for the posterior mandible with a remaining ridge height of 8–10 mm. b**, c**) A short dental implant is recommended. a***) A treatment option for the posterior mandible with a vertical bone height of more than 10 mm. b***, c***) Standard-length implants are recommended. Primary vertical bone augmentation followed by the placement of standard-length implant |
||
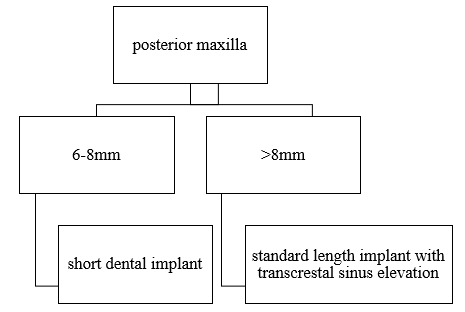
Short implants on maxilla
The physiological process of sinus pneumatization, particularly in the maxillary posterior region, exacerbates bone resorption. Therefore, bone quantity and quality is often insufficient for the ideal three-dimensional (3D) implant positioning [77]. Methods like for sinus augmentation with autogenous bone or sinus elevation to address poor bone height and enable the placement of standard implants. In individuals undergoing sinus floor elevation, consequences may include upper lip paresthesia, sinus membrane perforation, localised infection, edema, hematoma, and maxillary sinusitis. As a novel technique to facilitate implant placement in compromised alveolar bone while preventing possible damage to vital structures, short implants were introduced [3].
Yan et al. reviewed and concluded that short implants (≤6 mm) are a viable alternative for sinus floor elevation in cases with atrophic posterior maxilla, since they have a similar survival rate, lower MBL, and less postsurgical reactions [78].
Different treatment options includes [76] (Figure 6a, 6b),
|
|
|
|
|
a*) |
b*) |
c*) |
|
a) |
||
|
|
|
|
|
a**) |
b**) |
c**) |
|
b) |
||
|
Figure 6. a*) A treatment option for the posterior maxilla with a vertical bone height of more than 8 mm. b*, c*) A transcrestal sinus elevation approach can be chosen for a vertical ridge dimension exceeding 8 mm and if standard-length implants are the preferred option. a**) treatment option for the posterior maxilla with a vertical bone height of 6–8 mm. b**, c**) A short dental implant is recommended |
||
Results and Discussion
The length of the implant is a crucial decision that affects both the prosthesis's overall success and the implants' survival rates. Due to the low quality and amount of bone, implant placement in the posterior region of the maxilla and mandible has always been critical. Long implants can be placed in conjunction with complex surgical operations like bone augmentation and sinus lift. Therefore, in regions with low bone quantity and quality, a less invasive treatment alternative is required. Thus, short implants are starting to lead the way in implant dentistry. An increase in the bone implant contact area results from improvements to the implant's surface geometry and texture, which offers strong primary stability during osseo-integration.
Conclusion
The use of short dental implants has proven achievable in patients which are apprehensive in undergoing augmentation procedures of sorts. Treatment with short implants can be considered safe and predictable if used under strict clinical protocols in atrophic maxillary and mandibular atrophic ridges. Additional high-quality studies are needed to evaluate the long-term effectiveness of short implants regarding the implant location and its success rate.
Acknowledgments: None
Conflict of interest: None
Financial support: None
Ethics statement: None