Knowledge Of Antibiotics And Antimicrobial Resistance Among Clinical Dental Students In Riyadh & Eastern Region; A Survey-Based Study
Nawaf Alhamidi1, Nassr Aldajani1, Sultan Alqahtani1, Mohammed Altareef1, Ziyad Aalsaif1, Umbreen Noor2*
1 Medical Interns, Riyadh Elm University, College of Dentistry, Riyadh,Saudi Arabia.
2 Faculty of Dentistry, Lecturer of Anatomy and Physiology in Basic Sciences Department, Riyadh Em University, Riyadh, Saudi Arabia.
ABSTRACT
Background: Antibiotics as one of the major factors of life-expectancy increment, are prescribed for infectious diseases caused by bacteria. However, the world faced the most significant issue of antimicrobial resistance. Several studies have conducted to gauge the level of awareness about antibiotics microbial resistance (AMR). According to the sevral researches, 54% dentists overprescribe antibiotics, and one‐tenth of them believed that antibiotics should be used for the treatment of flu and the common cold.
Objective: The purpose of this study is to measure the knowledge of antibiotics and antimicrobial resistance among clinical dental students.
Method: A cross-sectional study was conducted among dental students in Riyadh and the Eastern region using an online survey. A total of 791 students participated in an online questionnaire consisted of demographic information followed by knowledge related questions about antibiotic prescription and bacterial resistance.
Conclusions: Antibiotics are highly used among dental students despite their good knowledge about antibiotics resistance. Female students showed better knowledge of an attitude towards the use of antibiotics as compared to males. 4th-year students showed better knowledge and attitude towards antibiotics resistance. There is a need to improve dental students' attitudes towards the use of antibiotics.
Key words: Antibiotics, microbial Resistance, Dental Students.
Introduction
Antibiotics are medicines that are prescribed for infectious diseases caused by bacteria and are a major factor that has increased the life expectancy of many. However, a major problem of antimicrobial resistance is now being faced by the world. The fast-evolving antibiotic resistance crisis jeopardizes the remarkable health advantages that have been accomplished through antibiotic medication. This resistance is not just a geographical threat but has become a worldwide problem. Another issue is the knowledge and information about these resistances, although the factor like the lifestyle that may lead to antibiotic/antimicrobial resistance but nearly all the knowledge regarding the antibiotics and AMR is limited in the English language, hence the penetration world over is very low 1, 2. Infectious diseases have always constituted the most serious health issue in the world. 3-6.
Around 90% of all antibiotic prescriptions are made in primary care, and a wide gap has been detected between standards and medical practice being carried out. Sources of information on antibiotics are an important determinant of the quantity and quality of antibiotic prescribing in primary care. The receipt of the information on AMR does not always guarantee an increase in awareness of antibiotic resistance. However, the least knowledgeable group having an indifferent world view are the most susceptible to have an increased awareness after the provision of such information. Other than lifestyle, misuse, and/or overuse of antibiotics is the main reason for the predicament of resistance 7, 8.
Another major cause of the antibiotic resistance crisis is overdosage and self-medication. It is without a doubt that the world is moving towards a post-antibiotic period where due to negligence or otherwise, common and minor infections and/or injuries have been for decades treated with the use of antibiotics. Now such infections are resurgent, stronger than ever which may again lead to widespread epidemics. The inappropriate usage of antimicrobial drugs and control methods adds further to its relapse 9, 10.
With the advancement of medical science, new antibiotics are being made every passing moment to provide us with a counter measure against the diseases. However, while prescribing these new antibiotics extreme caution should be taken as any improper use can lead to the emergence of new antimicrobial resistance for which there may be medicine available for curing. Therefore, the antimicrobial stewardship team (AST) and the commission of infections (CI) have a very crucial task of achieving the acceptable use of these newly discovered antibiotics 11.
Several studies have conducted to gauge the level of awareness about AMR, one of the study suggests that 54% dentists overprescribe antibiotics, and one‐tenth of them believed that antibiotics should be used for the treatment of flu and the common cold. In face of such a global issue, it is therefore of primary importance to further educating dental students about the antibiotics and risks associated with its misuse 12. Another study shows that the overall awareness about antibiotic use and understanding of AMR amongst students is higher in a developed country as compared to a developing country 13.
One of the studies signifies that the majority of the students believe that AMR is a preventable challenge but with appropriate strategies in place. Despite such a majority, they have poor knowledge regarding antimicrobial resistance. The study also suggests that improving the students’ level of knowledge about antibiotics and antimicrobial resistance should be a method to enhance their approach and to optimize rather than reduce or overuse of their antimicrobial prescription 14.
Study hypotheses:
Knowledge of clinical dental students about antibiotic resistance is satisfactory.
Aims of the study:
Materials and Methods:
Study Design: This is a cross-sectional study conducted among dental students in Riyadh and the Eastern region using an online survey.
Study Sample: All dental universities in Riyadh and the Eastern regions were contacted and 491 students filled up the survey.
Study Instrument: Online questionnaire was constructed which consisted of demographic information followed by knowledge related questions about antibiotic prescription and bacterial resistance.
Instrument Validity and Reliability: A pilot study was conducted by letting the survey be filled by 20 participants and the data was inserted in SPSS version 22 to determine the reliability by using Chronbach’s coefficient alpha (Value was .791). The validity of the questionnaire was tested by sending it to experienced researchers in REU and no changes were made.
Statistical Analysis: Collected data were analyzed using SPSS version 22, where descriptive as well as inferential statistics was conducted. Comparisons between groups were made with the value of significance kept under 0.05.
Results:
Results show 47% were males and 53% females (Fig 1), 44% belonged to 4th year, 23% to 5th year, and 33% from the final year (Fig 2). 47% had reported regular medication use, 55% had used antibiotics in the last 12 months. 90% of females believed antibiotics were beneficial, 88% of females thought antibiotics are overused, and 88% of females supported its restrictive use. 96% of females reported that bacteria can become resistant against antibiotics, 72% of females thought a patient can stop taking antibiotics when feeling better without completing the course.
As far as dentistry years were concerned, 91% of the 4th year students supported antibiotic’s restrictive use, 95% of the 5th year students believed one could get better from bacterial infections without the use of antibiotics. Only 33% of the final year student reported that antibiotics are effective against influenza. 96% of the 4th year students believed that resistant bacteria are becoming a common problem in Saudi Arabia. (Table 1)
Table 1: Queationaire results
|
Gender: Male Female |
292 (47%) 329 (53%) |
|
Dentistry Year: 4th Year 5th Year Final Year
|
275 (44%) 144 (23%) 202(33%)
|
|
I Have Good Health Strongly Agree Agree Unsure Disagree Strongly Disagree
|
398 (64%) 181 (29%) 28 (5%) 12(2%) 4(1%)
|
|
I Have Chronic Disease: Yes No Will Not Report
|
276 (44%) 329 (53%) 17(3%) |
|
Smoker: Yes No Sometimes
|
331 (53%) 257 (42%) 33(5%) |
|
Regular Medication Use: Yes No Sometimes
|
295 (47%) 303 (49%) 24(4%) |
|
Antibiotic Use in last 12 months: Yes No Don’t Remember
|
341 (55%) 243 (39%) 37(6%) |
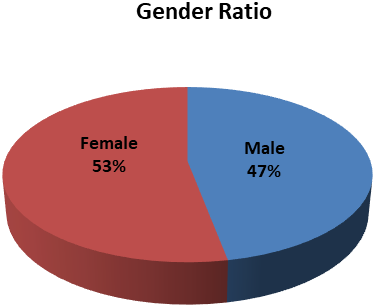
Fig. 1: Gender Ratio
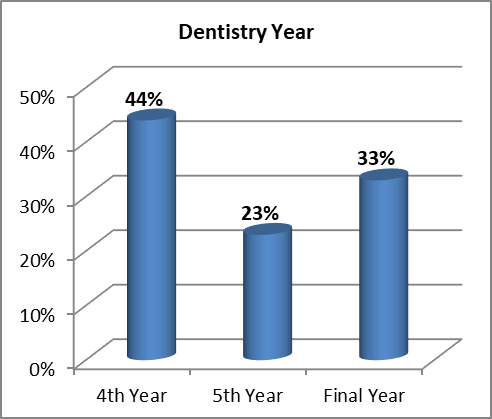
Fig. 2: Dentistry Year Distribution of Study Participants
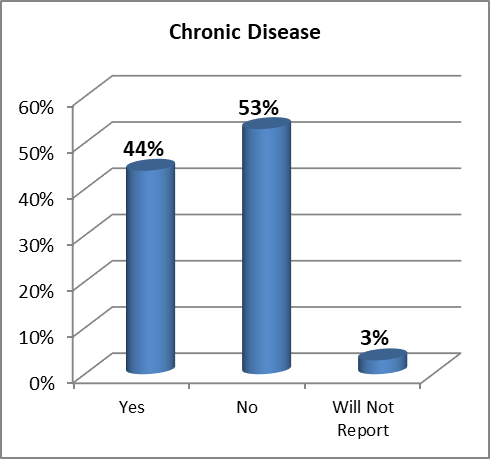
Fig. 3: Chronic Disease Distribution of Study Participants
Table 2: Comparison based on Gender
|
Item |
Male |
Female |
P-Value |
|
I Have Good Health |
Strongly Agree 52%
Agree 38%
Unsure 6%
Disagree 3%
Strongly Disagree 1% |
Strongly Agree 74%
Agree 22%
Unsure 3%
Disagree 1%
Strongly Disagree 0% |
0.000 |
|
I have Chronic Disease
|
Yes 29%
No 67%
Will No Report 4% |
Yes 59%
No 40%
Will No Report 2% |
0.000 |
|
Smoker
|
Yes 46%
No 45%
Sometimes 9% |
Yes 60%
No 38%
Sometimes 2% |
0.000 |
|
Regular Medication Use
|
Yes 31%
No 65%
Sometimes 4% |
Yes 62%
No 34%
Sometimes 3% |
0.000 |
|
Antibiotic Used In Last 12 Months
|
Yes %42
No 52%
Don’t Remember 6% |
Yes 67%
No 28%
Don’t Remember 6% |
0.000 |
|
Beliefs About Medicines |
|||
|
Beneficial
|
Agree 81%
Disagree 4%
Uncertain 15% |
Agree 90%
Disagree 1%
Uncertain 9% |
0.003 |
|
Harmful
|
Agree 70%
Disagree 11%
Uncertain 19% |
Agree 86%
Disagree 3%
Uncertain 11% |
0.000 |
|
Overused
|
Agree 75%
Disagree 9%
Uncertain 16% |
Agree 88%
Disagree 4%
Uncertain 8% |
0.000 |
|
Attitude About Antibiotics |
|||
|
Restrictive Attitude Supported
|
Agree 79%
Disagree 4%
Uncertain 18% |
Agree 88%
Disagree 1%
Uncertain 11% |
0.005 |
|
Non-Restrictive Attitude Supported
|
Agree 46%
Disagree 16%
Uncertain 39% |
Agree 67%
Disagree 5%
Uncertain 27% |
0.000 |
|
Antibiotics In General |
|||
|
Antibiotics will kill our beneficial bacteria on the skin or stomach/intestines |
True 88% |
True 98% |
0.000 |
|
You can get well from bacterial infections without antibiotics |
True 81% |
True 92% |
0.000 |
|
Antibiotics are effective against colds |
True 48% |
True 70% |
0.000 |
|
Other medications may influence the effect of antibiotics |
True 87% |
True 92% |
0.021 |
|
Antibiotics are effective against influenza |
True 48% |
True 70% |
0.000 |
|
You can take antibiotics together with all kinds of food |
True 49% |
True 70% |
0.000 |
|
ANTIBIOTICS RESISTANCE |
|||
|
Bacteria can become resistant against antibiotics |
True 90% |
True 96% |
0.002 |
|
Unnecessary use of antibiotics can make them less effective |
True 86% |
True 95% |
0.000 |
|
If you are well halfway through the antibiotics cure and feel well, you can stop the treatment. |
True 43% |
True 72% |
0.000 |
|
One can be a carrier of resistant bacteria without being sick |
True 81% |
True 93% |
0.000 |
|
Infections by resistant bacteria are increasing in Saudi Arabia |
True 90% |
True 94% |
0.109 |
|
Resistant bacteria are a problem at Saudi Arabian hospitals |
True 87% |
True 93% |
0.018 |
|
Humans can become resistant against antibiotics |
True 87% |
True 96% |
0.000 |
Table 3: Comparison of the Dentistry Year
|
Item |
4th year |
5th Year |
Final Year |
P-Value |
|
I Have Good Health |
Strongly Agree 77%
Agree 16%
Unsure 5%
Disagree 2%
Strongly Disagree 0% |
Strongly Agree 61%
Agree 31%
Unsure 5%
Disagree 2%
Strongly Disagree 1% |
Strongly Agree 49%
Agree 45%
Unsure 3%
Disagree 2%
Strongly Disagree 1% |
0.000 |
|
I have Chronic Disease
|
Yes 72%
No 25%
Will No Report 2% |
Yes 24%
No 71%
Will No Report 4% |
Yes 21%
No 77%
Will No Report 2% |
0.000 |
|
Smoker
|
Yes 70%
No 26%
Sometimes 4% |
Yes 42%
No 51%
Sometimes 7% |
Yes 39%
No 55%
Sometimes 6% |
0.000 |
|
Regular Medication Use
|
Yes 74%
No 24%
Sometimes 2% |
Yes 32%
No 62%
Sometimes 6% |
Yes 22%
No 73%
Sometimes 4% |
0.000 |
|
Antibiotic Used In Last 12 Months
|
Yes 78%
No 19%
Don’t Remember 3% |
Yes 38%
No 50%
Don’t Remember 12% |
Yes 36%
No 58%
Don’t Remember 6% |
0.000 |
|
Beliefs About Medicines |
||||
|
Beneficial
|
Agree 92%
Disagree 1%
Uncertain 7% |
Agree 80%
Disagree 6%
Uncertain 15% |
Agree 82%
Disagree 2%
Uncertain 15% |
0.001 |
|
Harmful
|
Agree 89%
Disagree 5%
Uncertain 7% |
Agree 76%
Disagree 6%
Uncertain 18% |
Agree 65%
Disagree 11%
Uncertain 24% |
0.000 |
|
Overused
|
Agree 88%
Disagree 4%
Uncertain 8% |
Agree 74%
Disagree 10%
Uncertain 16% |
Agree 80%
Disagree 7%
Uncertain 12% |
0.008 |
|
Attitude About Antibiotics |
||||
|
Restrictive Attitude Supported
|
Agree 91%
Disagree 1%
Uncertain 8% |
Agree 80%
Disagree 2%
Uncertain 18% |
Agree 76%
Disagree 5%
Uncertain 20% |
0.000 |
|
Non-Restrictive Attitude Supported
|
Agree 76%
Disagree 4%
Uncertain 20% |
Agree 59%
Disagree 8%
Uncertain 33% |
Agree 31%
Disagree 21%
Uncertain 49% |
0.000 |
|
Antibiotics In General |
||||
|
Antibiotics will kill our beneficial bacteria on the skin or stomach/intestines |
True 95% |
True 93% |
True 91% |
0.338 |
|
You can get well from bacterial infections without antibiotics |
True 92% |
True 95% |
True 83% |
0.003 |
|
Antibiotics are effective against colds |
True 78% |
True 58% |
True 36% |
0.000 |
|
Other medications may influence the effect of antibiotics |
True 93% |
True 85% |
True 88% |
0.013 |
|
Antibiotics are effective against influenza |
True 79% |
True 59% |
True 33% |
0.000 |
|
You can take antibiotics together with all kinds of food |
True 79% |
True 62% |
True 34% |
0.000 |
|
ANTIBIOTICS RESISTANCE |
||||
|
Bacteria can become resistant against antibiotics |
True 95% |
True 90% |
True 93% |
0.122 |
|
Unnecessary use of antibiotics can make them less effective |
True 96% |
True 86% |
True 87% |
0.000 |
|
If you are well halfway through the antibiotics cure and feel well, you can stop the treatment. |
True 78% |
True 60% |
True 32% |
0.000 |
|
One can be a carrier of resistant bacteria without being sick |
True 91% |
True 82% |
True 86% |
0.050 |
|
Infections by resistant bacteria are increasing in Saudi Arabia |
True 96% |
True 90% |
True 89% |
0.011 |
|
Resistant bacteria are a problem at Saudi Arabian hospitals |
True 94% |
True 89% |
True 86% |
0.011 |
|
Humans can become resistant against antibiotics |
True 94% |
True 85% |
True 93% |
0.005 |
Discussion
This study was conducted to assess the knowledge of antibiotics and antimicrobial resistance among clinical dental students in Riyadh & the Eastern region. A total of 621 dental students participated in the survey and provided the needed insight into the subject matter. The students chosen were from 4th to final year of dentistry. 64% of the respondents said that they believe that they have good health, however, 44% of the students said that they suffer from some form of chronic disease. (Fig 3) It is pertinent to note 53% of the students said that they smoked regularly. A high percentage (47%) of the students used medicine regularly and most of them (55%) had used an antibiotic in the last 12 months. table (3). In another study, similar results were found where 57.7% of the respondents had taken antibiotics in the last 12 months 15.
The results were also compared against students’ gender and the years spent in the dentistry college as well to assess if any statistically significant incidences exist for the furtherance of this research.
As far as gender is concerned, statistically significant differences were found, that the female gender was more inclined towards, when inquired about having good health (p-value: .000), having the chronic disease (p-value: .000), regularly smoking (p-value: .000), regular usage of any medication (p-value: .000) and taking an antibiotic in the last 12 months (p-value: .000). table (2).
The female gender also thought that the medicines are beneficial (p-value: .003) and they do have harmful effects as well (p-value: .000) they also thought that medicines are often overused (p-value: .000), more than the male gender, as statistically significant differences were found in these results. table (2).
The awareness of the female gender was also higher when asked about their attitude about antibiotics, and they supported a restrictive attitude towards antibiotics (p-value: .005) and also supported non-restrictive attitude (p-value: .000). table (2). These results are similar to another study where it was shown that the Male gender has a less restrictive attitude toward antibiotic use 16.
Also, they showed more knowledge when inquired about antibiotics in general, whether Antibiotics also kill beneficial bacteria on the skin or stomach/intestines (p-value: .000), whether one can get well from bacterial infections without antibiotics (p-value: .000), whether Other medications may influence the effect of antibiotics (p-value: .021), whether one can take antibiotics together with all kinds of food (p-value: .000). However, the female gender was more inclined to misuse as compared to male as they erroneously answered when inquired whether antibiotics are effective against colds (p-value: .000), whether antibiotics are effective against influenza (p-value: .000), table (2)
The female gender as compared to male gender also showed more awareness about antibiotics resistance as statistically significant differences were found when asked whether bacteria can become resistant against antibiotics (p-value: .002) table (2). and that unnecessary use of antibiotics can make them less effective (p-value: .000) table (2). whether if one is well halfway through the antibiotics cure and feel so, he/she can stop the treatment (p-value: .000) table (2). that one can be a carrier of resistant bacteria without being sick (p-value: .000) table (2). Females in the survey also think that resistant bacteria is a problem at Saudi Arabian hospitals (p-value: .000) table (2).and that humans can become resistant against antibiotics (p-value: .000) table (2).
In another study conducted it showed that 76.9% of the people would choose the antibiotic-free option as they showed awareness for the harmful effects of its usage 17.
When assessed against the number of years spent in the dentistry college, the students in the 4th year thought that the medicines are beneficial (p-value: .001) table (3). and they do have harmful effects as well (p-value: .000) table (3). they also thought that medicines are often overused (p-value: .008) table (3). more than students of 5th or final year, as statistically significant differences were found in these results. table (3).
The awareness of 4th-year students was also higher when asked about their attitude about antibiotics, and they supported a restrictive attitude towards antibiotics (p-value: .000) and also supported non-restrictive attitude (p-value: .000). table (3). Also, they showed more knowledge when inquired about antibiotics in general, whether one can get well from bacterial infections without antibiotics (p-value: .003) table (3). whether Other medications may influence the effect of antibiotics (p-value: .013) table (3). whether one can take antibiotics together with all kinds of food (p-value: .000). table (3). The 4th year students also erroneously answered when inquired whether antibiotics are effective against colds (p-value: .000) table (3). and whether antibiotics are effective against influenza (p-value: .000). table (3). In a similar study, 30% of the students stated that antibiotics are effective against viruses, cold, and influenza 16.
The 4th year students as compared to 5th or final year students also showed more awareness about antibiotics resistance as statistically significant differences were found when asked that unnecessary use of antibiotics can make them less effective (p-value: .000) table (3). whether if one is well halfway through the antibiotics cure and feel so, he/she can stop the treatment (p-value: .000) table (3). that one can be a carrier of resistant bacteria without being sick (p-value: .050) table (3). 4th-year students in the survey also think that resistant bacteria is a problem at Saudi Arabian hospitals (p-value: .011) table (3). and that humans can become resistant against antibiotics (p-value: .005) table (3). In one of the studies carried out, the students in a dental college were found to be not aware of the antimicrobial resistance 18.
Conclusions:
References
Corresponding Author
Umbreen Noor
Faculty of Dentistry, Lecturer of Anatomy and Physiology in Basic Sciences Department, Riyadh Em University, Riyadh, Saudi Arabia.
Email: umbreennoor.muhammad @ riyadh.edu.sa