INFLUENCE OF BACKGROUND AND CEMENT SHADES ON THE COLOR OF HIGH-TRANSLUCENCY LITHIUM-DISILICATE CERAMICS
Mohammed Zahran1, Dania Sabbahi2, Ahmed Alghamdi3, Ahmed Al-Otaibi4, Bashayer Altaefi1, Lina Baessa5, Lalyan Bahha3
1 King Abdulaziz University, Faculty of Dentistry, Oral and Maxillofacial Prosthodontics Department, 3527 Abdullah Alsulaiman St., Jeddah 22252, Saudi Arabia.
2King Abdulaziz University, Faculty of Dentistry, Dental Public Health Department, 3527 Abdullah Alsulaiman St., Jeddah 22252, Saudi Arabia.
3 Private Practice, Jeddah, Saudi Arabia.
4 Private Practice, Riyadh, Saudi Arabia.
5 King Abdulaziz University, Faculty of Dentistry, Orthodontic Department, 3527 Abdullah Alsulaiman St., Jeddah 22252, Saudi Arabia.
|
|
INTRODUCTION
Nowadays, esthetic dental treatment is a lot more challenging for dentists due to higher patients’ expectations regarding the esthetic outcome 1. Increasing demand for highly esthetic restoration is due to the evolution of social media and increased awareness regarding dental treatment options. One of the most challenging situations is matching the shade of an artificial anterior restoration with those of adjacent natural teeth 2. This can be even more challenging when having a combination of natural teeth and implant-supported restorations due to the different background colors. Implant-supported restorations were used to be quite challenging in the past, because of the titanium abutment that imparts a darker shade to the ceramic restoration. In contemporary, with the advancement in ceramics, yttrium-stabilized zirconium oxide polycrystals (Y-TZP) materials are taking over the titanium abutment yielding in a better shadowing effect to the ceramic restoration 3,4.
The innovation of ceramic technology had prompted industries to develop new materials with superior optical and mechanical properties. Lithium disilicate is one of the most commonly used among dental ceramics as they provide optimal translucency aiding in a better light transmission thought the restoration in addition to their high mechanical properties 5. Matching ceramic restorations made using these translucent ceramics with natural teeth is very challenging and cannot be ensured 6, especially when cemented to natural teeth and/or implant-supported abutments with different stump shades.
Multiple factors might affect the final color of ceramic restorations. These factors can be divided into three main categories: substrate-related, cement-related, and ceramic-related 7, 8. It has been suggested in previous studies that darker background (e.g. non-vital teeth, implant titanium abutments, or dark shade core build-ups) would result in a darker final restoration, and vice versa 3, 6, 9. Another factor is ceramic thickness which may affect both ceramic translucency and color, therefore this factor can be helpful when trying to mask a darker substrate 2, 4, 6. Several studies evaluated the effect of luting cement shade as a factor contributing to the final restoration color, and it has been concluded that the opaquer the shade of luting cement, the greater the ability to mask the underlying dark substrate 2, 10.
Colorimetry in dentistry elaborated on the Commission Internationale de l'Eciairage (CIE) method, which explains the relationship between color difference and their perception and acceptance in clinical practice, besides, determining a translucency parameter 11. These parameters play a role in inherited optical properties for dental material, and their integration together has an advantageous outcome concerning esthetics.
Thus, the purpose of this in-vitro study was to determine the color difference using the diversity of background shades and resin luting cement and their implication to approximately approach clinical reality. The null hypothesis was that there is no significant effect of the background shade and luting cement shade and their interaction on the color of high translucent lithium disilicate ceramic.
MATERIALS AND METHODS
All the materials used in the study and their specifications were listed in Table 1.
Specimen Preparation
Sixty high translucent lithium-disilicate glass-ceramic (HT-LDGC) rectangular specimens were sectioned from a pre-sintered (IPS-e.max®CAD blocks (size C14), Ivoclar/Vivadent, Liechtenstein) into 1.4±0.2 mm thickness using a diamond wafering blade (UKAM Industrial Superhard Tools Valencia, USA) on a slow-speed saw (Isomet 2000 Precision Saw, Buehler, USA). After sectioning, samples were crystallized using Programat® EP 3010 (Ivoclar/Vivadent). HT-LDGC samples were randomly divided into 12 groups based on the use of 4 background materials and the 3 cement shades.
Background specimens were fabricated using 4 different materials. The A2 and zirconia (ZR) specimens were sectioned from composite blocks (Lava Ultimate, 3M ESPE, Germany) and Y-TZP blocks (IPS e.max ZirCAD, Size C15, Ivoclar/Vivadent, Lichtenstein), respectively, similar to the HT-LDGC specimens. ZR specimens were sintered in a high-temperature furnace (Sintramat, Ivoclar Vivadent) following the manufacturer’s instructions. A composite core build-up material (LuxaCore Z-Dual, DMG, Germany) was used to fabricate background specimens with A3 and light opaque (LO) shades. The A3 and LO specimens were fabricated using a custom mold that was created using putty PVS material (Take 1 Advanced™ Putty, Kerr Corp., USA). The LuxaCore material was injected in the custom mold and then cured using LED curing light (Bluephase N, Ivoclar/Vivadent) for a total of 40 seconds (20sec/side). All background specimens were fabricated with 1.5 mm thickness. The thickness of ZR specimens was increased during sectioning by 25% to compensate for the shrinkage that is expected to take place during sintering, to achieve a final thickness of 1.5 mm.
All samples were polished using sandpaper with different grit sizes (220, 320, 400, and 600). The thickness of each specimen was verified using a digital caliper (Mitutoyo Corporation, Tokyo, Japan) before the cementation process. The HT-LDGC and zirconia samples were polished before crystallization/sintering.
All samples were polished using sandpaper with different grit sizes (220, 320, 400, and 600). The thickness of each specimen was verified using a digital caliper (Mitutoyo Corporation, Tokyo, Japan) before the cementation process. The HT-LDGC and zirconia samples were polished before crystallization/sintering.
Cementation Procedures
The four background groups (A2, A3, LO, and ZR) were cemented to their corresponding HT-LDGC specimen using self-adhesive dual-cure resin cement (Maxcem Elite Chroma, Kerr, U.S.A) with three different shades (clear, white, and yellow).
To standardize the cement layer thickness, a standardized weight of 64g was applied over the ceramic/background complex during cementation, followed by light curing using an LED light cure unit (Bluephase N, Ivoclar/Vivadent,) for a total of 40 seconds (20 sec/side).
Spectrophotometric Measurement
A digital spectrophotometer (VITA Easyshade; VITA Zahnfabrik, Bad Säckingen, Germany) was used to record the color coordinates in the CIE (Commission International de l’Eclairage) Lab color space system. A custom-made square box of 6 cm3 lined with a black interior with an opening hole in the top of the box to accommodate the tip of the spectrophotometer during measurement.
Two spectrophotometric readings were recorded for each specimen, for ceramic specimens alone (S1) as a baseline and the ceramic-background complex after cementation (S2), respectively. All recorded data were organized and tabulated in an excel sheet (Microsoft Excel for Mac, version 16.10, 2017) to be prepared for statistical analysis.
|
Material and Manufacturer |
Lot No. |
Shade |
Type |
|
LuxaCore Z-Dual (LO) (DMG, Germany) |
763208 |
Light opaque |
Composite core build-up material (Barium glass in a Bis-GMA resin matrix) |
|
LuxaCore Z-Dual (A3) (DMG, Germany) |
779562 |
A3 |
|
|
IPS-e.max ZirCad (ZR) (Ivoclar/vivadent, Liechtenstein) |
L13763 |
White |
Yttrium-stabilized zirconium-oxide |
|
Maxcem Elite Chroma (Kerr, U.S.A) |
6160098 |
White, clear and yellow |
Self-adhesive dual-cure resin cement |
|
LavaTM Ultimate (A2) (3M ESPE, Germany) |
N438267 |
A2 |
Nano-ceramic resin (Zirconia/silica fillers) |
|
IPS-e.max CAD HT (Ivoclar/vivadent, Liechtenstein) |
U23899 |
A3 |
Lithium-disilicate glass-ceramic |
Table 1. Characteristics of the materials used in this study.
To determine the effect of changing the background and the shade of the cement, color difference was calculated using the CIEDE2000 (DE00) according to the following formula:
∆E00=∆L'KLSL2+∆C'KCSC2+∆H'KHSH2+RT ∆C'KCSC∆H'KHSH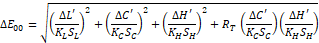
where ∆C′, ∆L′, and ∆H′ are the differences in chrome, lightness, and hue and where RT is a rotational function that accounts for the interaction between chroma and hue differences in the blue region. Weighting functions, SL, SC, and SH, adjust the total color difference for variation in the location of the color difference pair in L, a, b coordinates, and the parametric factors KL, KC, and KH are correction terms for experimental conditions.
The parametric factor of the CIEDE2000 color-difference formula was set to 1. While, the perceptibility threshold was set at ∆E00 =1.30 units, and the clinical acceptability threshold was set at ∆E00 >2.25 12, 13.
Statistical Analysis
Two-way ANOVA, followed by Tukey’s post hoc comparisons, was used to evaluate the effect of the background color, cement shade, and their interaction on the color difference (DE00). All statistical analyses were conducted using the SPSS software for Windows (version 20, SPSS Inc., IBM, Somers, New York, USA) at a significance level of 0.05.
RESULTS
Two-way ANOVA revealed significant effects of the background, cement shade, and their interaction on the color difference (Table 2). The mean color differences (DE00) of different groups in comparison to the baseline measurement are reported in Table 3. The reported DE00 values ranged between 1.6 to 9.1. Most of the groups showed DE00 values higher than clinically acceptable level (DE00 >2.25). Only two groups of the combination of LO background and clear cement and combination of zirconia background and yellow cement showed mean DE00 values within the clinically acceptable level (1.3 < DE00 ≤ 2.25).
|
Source |
Type III Sum of Squares |
df |
Mean Square |
F |
Sig. |
|
Corrected Model |
343.608 |
11 |
31.237 |
20.709 |
<0.001 |
|
Intercept |
1550.925 |
1 |
1550.925 |
1028.217 |
<0.001 |
|
Background |
269.290 |
3 |
89.763 |
59.511 |
<0.001 |
|
Cement |
25.194 |
2 |
12.597 |
8.352 |
0.001 |
|
Background * Cement |
49.123 |
6 |
8.187 |
5.428 |
<0.001 |
|
Error |
72.401 |
48 |
1.508 |
||
|
Total |
1966.935 |
60 |
|||
|
Corrected Total |
416.009 |
59 |
R Squared = 0.826 (Adjusted R Squared = 0.786)
Table 2. Two-way ANOVA (dependent variable: DE00; independent variables: background and cement shade).
|
Background |
Cement Shade |
||
|
Clear |
White |
Yellow |
|
|
A2 |
5.6 (1.8) c,d,e |
4.8 (1.2) b,c,d |
7.8 (0.7) e,f |
|
A3 |
7.0 (1.9) d,e,f |
7.9 (2.0) e,f |
9.1 (0.9) f |
|
LO |
1.6 (0.7) a |
5.0 (1.5) b,c,d |
4.5 (0.7) b,c,d |
|
ZR |
2.5 (0.7) a,b |
3.4 (0.4) a,b,c |
1.7 (0.7) a |
Results of Tukey post hoc comparisons are shown as superscript letters, and values having the same superscript letters were not significantly different (P>0.05).
Table 3. Mean (SD) for DE00 for the groups in the study.
DISCUSSION
The result of the present study suggests that the color perception of different background/cement shade combinations showed a statistically significant difference among the tested groups. Therefore, the null hypothesis was rejected.
The finding of the current study revealed lower DE00 for the samples fabricated using ZR and LO backgrounds in comparison to the samples fabricated using A2 and A3 backgrounds. This can be attributed to the white color of the ZR and LO backgrounds which reflect all the light that passes through the high-translucent lithium disilicate ceramic in comparison to the dark backgrounds (A2 and A3) which absorb more and reflect less light. This finding is in agreement with previous studies 3, 10.
In the present study, the best combinations that revealed the lowest color differences were LoC with HT-LDGC and ZrY with HT-LDGC, with DE00 of 1.6 and 1.7, respectively. These groups showed a clinically acceptable difference. The rest of the groups showed a significantly high mean DE00 values that detected easily as clinically unacceptable (DE00 >2.5). One possible explanation can be attributed to the high translucency of the lithium disilicate as it comprises a combination of the glass matrix and the lithium disilicate crystalline phase. This high translucency allows the light to pass through ceramic without scattering. The passing light will subsequently reflect the underlying background color 2.
The use of high and low translucent ceramics is challenging in cases that involve abutments with a variety of stump shades since they have limited ability to mask the underlying substructure 14, 15. In these challenging cases, the use of high opacity (HO) and medium opacity (MO) as core structure veneered by translucent veneering porcelain can be considered to provide better masking for the underlying structure and allow better shade matching 2.
Jirajariyavej et al. evaluated the effect of varying the ceramic thickness on the final color of different ceramics and concluded that increasing the ceramic thickness to 2.5 mm significantly decreased the color mismatch 4. In the present study, the thickness of ceramic samples was chosen to reflect the recommended thicknesses for the all-ceramic lithium disilicate crowns. Increasing the ceramic thickness to more than 1.5 mm might not be feasible in lots of situations and will contradict the concepts of conservative dentistry.
In the present study, changing the cement shade did not mask the effect of the background color but helped in tuning it. Adding white or clear shade to the dark backgrounds (A2 and A3) reduced the color difference while adding clear cement to LO or yellow cement to ZR background helped in tuning the color difference down. These findings are similar to the result reported in a previous study 4. Three different shades of cement were used in the current study (yellow, clear, and white), which represents the variety of dual-cure cement provided by different manufacturers. It is not clear whether varying the cement brand might change the results of the study. This can be the focus of future studies.
A previous study concluded that the use of zirconia abutment to support implant-supported lithium disilicate crowns was the most clinically accepted solution especially in areas of high esthetic demand when compared to titanium abutments 1. The result of our study suggests that matching the implant-supported crowns under white zirconia abutment with the adjacent natural or restored teeth might be challenging. One of the suggested solutions to overcome this challenge is using different shade for the zirconia abutment. As we point from our study, the use of yellow cement with a white zirconia substrate minimizes the color difference.
CONCLUSION
Within the limitation of this study, it seems that matching the color of adjacent HT-LDGC restorations is a difficult task. Varying the cement shade did not help in reducing the color difference between the background groups to a clinically acceptable level. Further investigations should be directed toward utilizing different LDGC translucencies and different zirconia shades.
ACKNOWLEDGMENT
The authors acknowledge and thank Saudi Dental Research (SDR) and Advanced Technology Research Lab (ATRL) at the Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia for their logistic and technical support.
REFERENCES
Corresponding Author
Mohammed Zahran
P.O. Box 126543
Jeddah 21352
Saudi Arabia
Email: mzahran @ kau.edu.sa