Mandibular Implant-Supported Precision Attachment-Retained Fixed Prosthesis: Case Report
Muhammet Emin Aksan DDS, PhD1, Ali Can Bulut DDS, PhD2*
1 Private Prosthodont, İstanbul, Turkey.
2 Department of Prosthodontics, Faculty of Dentistry, University of Kırıkkale, Kırıkkale, Turkey.
ABSTRACT
Background: A common clinical problem confronting prosthodontists is the design and maintenance of edentulous mandibular by the fixed implant-supported prosthesis.
Purpose: Aim of the paper is to study and describes the rehabilitation of a patient with edentulous mandible via precision attachment-retained implant-supported fixed prosthesis to compensate for the effect of mandibular deformation.
Materials and Methods: In one patient scheduled for the implant-supported prosthetic substructure was divided into three parts, the interforaminal region, and the posterior segments were not connected rigidly, but by a precision, attachment reducing the tension that can occur around the implant by increasing the precision and passive fit.
Results: Two years after the delivery of the prosthesis to the patient, the fit of the substructure and, the bone adaptation around the implant were observed not to have deteriorated in the radiograph.
Conclusions: Precision attachment-retained mandibular implant-supported fixed prosthesis used in an edentulous patient is a good alternative to reduce mandibular deformation and provide good stabilization and retention.
Key words: Implant, Fixed Prosthesis, Mandibular.
Introduction
Rehabilitation of a patient with edentulous mandibular by fixed implant-supported prosthesis with appropriate biomechanical and prosthetic principles is one of the goals of dental implant researches 1, 2. When the one-piece complete arch prosthesis is used for the rehabilitation of edentulous mandibular, the implants are tightly connected by a prosthesis without shock-absorbing capacity at the bone-implant interface and the implants placed posterior to the mental foramen have a higher risk of failure when compared to the anterior counterparts due to the possible mandibular flexion 2-4. The mentioned failure can result in bone loss especially around the implant, loss of implant fixation, torque loss in the superstructure screw, restoration fracture, or loss of restoration retention 5, 6. A possible cause of this condition is the mandibular deformation 7, 8. Median mandibular flexure (MMF) is the mandibular deformation characterized by the property of the mandible to flex inward during opening and protrusion movements of the jaw with a reduction in the width of the mandibular arch. These movements result from the contraction of the pterygoid muscles in the frontal plane of the mandible 9-11. The lateral component of pterygoid muscles determines the amount of the decrease in the width of the mandibular arch through an estimated load of 10N to 20N during the opening and closing movements 12-14. These small loads are directly transmitted to the bone in the peri-implant region and can be converted to high-stress concentration due to the splinting effect of a full-arch prosthesis without the ability to damp forces 15. Thus, the mandibular deformation considered to be insignificant and ruled-out in practice emerges as an important factor that may affect biomechanical behavior, passive fit, and long-term prognosis 16, 17.
Mandibular flexion must be considered to obtain long-term outcomes in implant-supported prostheses 6, 18, 19. Various mandibular fixed implant-supported prosthesis designs have been suggested to improve the stress distribution resulting from mandibular flexion 19-23. This case report describes the rehabilitation of a patient with edentulous mandible via precision attachment-retained implant-supported fixed prosthesis to compensate for the effect of mandibular deformation.
Case report
A 54-year-old male patient was consulted to the Faculty of Dentistry of Kırıkkale University, for assessment and manufacture of a mandibular fixed implant-supported prosthesis.24-27 Intraoral and radiological examination of the patient was performed and the lower jaw was observed to be completely edentulous and only the anterior teeth were found to be present on the upper jaw (Figure 1).

Figure 1: Initial panoramic X-ray.
Methods
The patient was free from any illness and medication according to his medical history. Following the intraoral evaluation, the proposed treatment was the installation of 6 osseointegrated implants (10 × 4.5 mm; Oxy Implant Dental System, Italy) considering the bone volume of the patient. After the surgical stage, a temporary, heat-polymerized, complete prosthesis, preoperatively manufactured, was loaded by using a soft lining. The soft lining material was replaced every 15 days until the prosthetic stage (during 3 months). Two weeks before the prosthetic stage, the implants were surgically exposed, the healing abutments were screwed and, the temporary complete prosthesis was fitted to the soft lining material.
In the prosthetic stage, firstly impression was made with a polysiloxane impression material (Optosil Comfort Putty, Xantopren VL Plus; Heraus Kulzer, Germany) using the plastic impression copings via prefabricated tray (Figure 2). A multiunit abutment was placed on the mold (stone model) obtained with the initial impression. The abutments were then connected with dental floss and supported with auto polymerizing resin (GC pattern resin; GC America Inc.). The interfaces were then cut with a diamond disk cutter.
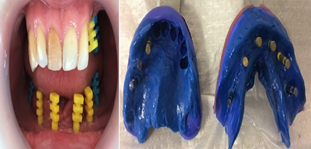
Figure 2: Impression procedure
Then, these pieces were re-integrated in the mouth with the same resin. This method allows an accurate transfer of the relation and position of the implants to the master model 19, 22. To reduce the ultimate impression stress, the mouth opening at the physiological rest position16 was measured with an individualized open tray by using medium-viscosity polyether without an increase in the mouth opening (Impregum Penta; 3M ESPE) and, type IV gypsum was used for casting (Prima-rock; Whip Mix Corp). After the centric relationship was recorded, the models were connected to the articulator.
During substructure waxing, a patrix was attached to the distal portions of the implant-supported fixed prosthesis located at the front region. Thus, the prosthesis structure was composed of three parts supported by the most distant implant parts and made of Cr-Co by conventional casting after waxing (Figure 3).

Figure 3: Metal framework
Precision attachments were made of metal-metal composition. Once the anterior part of the substructure was installed and the terminal screw on the right side was tightened, the clinical and radiological evaluation was performed. The same process was repeated for the left side 21, 23. Then the other parts were placed separately, the terminal screws were tightened and the whole substructure was evaluated in clinical and radiological aspects. In the end, the passive fit was checked 21. The porcelain superstructure was constructed following the evaluation of the substructure and was tried on the chairside (Figure 4).

Figure 4: Restorations after veneering.
The form of the teeth and the occlusion were assessed chairside (Figure 5) and the restoration was controlled by panoramic radiography (Figure 6). The patient was satisfied with the function and phonation.
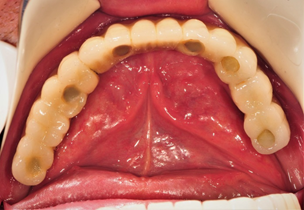
Figure 5: Finished the metal-ceramic crowns.

Figure 6: Finished mandibular metal-ceramic crowns; panoramic x-ray view.
Results
At two years, following the installation of the prosthesis, no complaint, porcelain fracture, screw loosening, or loss of posterior implants were reported (Figure 7-8).

Figure 7: Panoramic radiograph at 2-year recall.
The fit of the substructure and, the bone adaptation around the implant were observed not to be deteriorated in the panoramic radiogram (Figure 8).

Figure 8: Intraoral facial view at 2-year recall.
Clinically, no ceramic fracture, screw loosening, or fracture was found. The patient was satisfied with the prosthesis within 2 years and did not experience any aesthetic, function, or phonation loss. However, the use of the CAD/CAM technique instead of the casting technique for the design of this prosthesis during the production process could be tried in the context of passive fit increment and for ease 16, 17. However, that approach was not preferred as it included a considerable high cost.
Discussion
From a mechanical point of view, one of the main purposes of implant therapy is to provide low-stress implant-supported restoration.1 The stress of the lower jaw concentrates on the implants in the posterior region because mandibular deformation is more effective in the molar region than in the interforaminal region (canine and premolar region). Also, it was reported in the literature that the distribution of the tension during unilateral molar chewing was better in the prostheses that were separated into three parts posterior from the interforaminal region than the prostheses that were divided into two parts along the midline 5. Therefore, in this case, the implant-supported prosthetic substructure was divided into three parts, the interforaminal region, and the posterior segments were not connected rigidly, but by a precision, attachment reducing the tension that can occur around the implant by increasing the precision and passive fit. Furthermore, mandibular deformation has been mentioned as a parameter to be considered in implant-supported prosthesis design in several studies 1, 6, 18, 20. In a clinical case, to prevent mandibular deformation of the metal-based acrylic prosthesis, the substructure was separated into three parts from the posterior interforaminal region with the aid of a separator 21. The fragmentation of the prosthetic substructures in the lower jaw has been recommended in various studies1, 19-21 as it allows the mandibular flexion to be similar to its natural state 17, 23.
Mandibular flexion is a multifactorial phenomenon. The quality and quantity of the bone, the number and location of the implants, the measurement technique, and the design of the prosthesis are factors affecting this phenomenon 16, 17. In particular, to minimize the tension at the time of measurement, the measure of the mouth opening of the patient may be taken not to exceed 20 mm in the physiological rest position to reduce mandibular deformation. The prosthesis design can be composed of two or three parts or a non-rigid connector can be used 16. Therefore, the reduction of the mandibular deformation with the measurement technique and the prosthesis design was targeted in our case.
In this case, the effect of occlusion in the posterior region was increased and the lever arm was tried to be reduced by implant installation to the posterior region to the interforaminal region. In this case, a better distribution of occlusal forces was achieved 21. Also, by connecting the implants posterior to the interforaminal region to the anterior part by precision-attachments, a force-breaking effect and, the reduction of a possible effect of mandibular deformation were aimed. This implant-supported fixed prosthesis was prepared by considering biomechanical properties with a novel design involving different geometries from the successfully applied Brenemark protocol.
Conclusion
The precision attachment-retained mandibular implant-supported fixed prosthesis used in an edentulous patient is a good alternative to reduce mandibular deformation and provide good stabilization and retention. However, prospective follow-up sessions are required and the long-term success of the prosthesis should be investigated.
Conflict of Interest Statement
No conflict of interest
Author Contribution Statement:
All authors' are equally contributed to the article.
References
Corresponding Author
Dr. Ali Can Bulut
Department of Prosthodontics, Faculty of Dentistry, University of Kırıkkale, Kırıkkale, Turkey.
Email: alicanbulut @ outlook.com
Tel: 00 90 318 2244927