EFFECT OF LUTING AGENT ON THE LOAD-BEARING CAPACITY OF MILLED HYBRID CERAMIC SINGLE-TOOTH RESTORATION
Hanin Essam Yeslam1*, Abrar Kheder Aljadaani2, Alanoud Meteb Almalky3, Majed Mohammad Zahran2, Fatin Abdulrahman Hasanain1
1Department of Restorative Dentistry, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia. [email protected]
2Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia.
3Ministry of Health, Tabuk, Saudi Arabia.
https://doi.org/10.51847/l0X0mVhoeA
ABSTRACT
Hybrid ceramics offer a strong combination of ceramics and resin polymers for dental restorations. Choosing the right luting agent is crucial for their longevity and load-bearing ability. This study aimed to examine how different luting agents affect the load-bearing capacity of CAD/CAM milled hybrid ceramic crowns. CAD/CAM VITA Enamic hybrid ceramic blocks were used to create 15 identical crowns, which were divided into 3 groups and cemented with different luting agents: dual-cure resin, light cure resin, and glass ionomer cement (GIC). Pre-prepared polyurethane resin abutments with periodontal ligament simulation were used and mounted on a universal testing machine to measure maximum loads at fracture. Results were compared using ANOVA (p< 0.05). Although there was no statistically significant distinction in the maximum load at fracture between the groups, resin luting gels demonstrated higher loads than glass ionomer. As seen through visual inspection, GIC displayed more catastrophic fractures in the crowns than resin. The impact of luting agent type on CAD/CAM crown fracture loads appears to be minimal. However, evidence suggests that resin may be a more favorable option than GIC.
Key words: Restorative dentistry, Hybrid ceramic, Luting agent, Fracture load, CAD/CAM, Composite Resin.
Introduction
Recent advancements in dental technology have made it possible to create dental restorations that look natural, are long-lasting, and are biocompatible [1]. Non-metallic esthetic computer-aided design/computer-aided manufacturing (CAD/CAM) materials like ceramics and composites have become popular in dentistry over the last few years [2]. Glass and feldspathic ceramics can be brittle and prone to fracture, causing wear on opposing teeth and requiring precise handling during dental procedures [3]. All-ceramic restorations may break due to imperfections in the intaglio surface, which can cause small cracks to grow faster intraorally [4]. This can result in the need to replace them if the ceramic veneer chips or if the whole restoration breaks completely [5, 6]. Compared to ceramics, resin-based materials that are more flexible are better shock absorbers. However, they tend to have lower strength and durability. In the world of CAD/CAM, there are now hybrid ceramics including resin-reinforced ceramic materials that combine the advantages of both polymers and ceramics [7]. This eliminates the necessity for a final firing stage, allowing for quicker and more precise restorations [8]. There are currently two types of hybrid ceramics available for CAD/CAM fabrication of definitive indirect single-tooth restorations (crowns): polymer-infiltrated ceramic network (PICN) materials and materials with dispersed fillers [9]. Both materials have an elastic modulus closer to that of dentin and can absorb masticatory forces, making them especially useful for implant-supported restorations [9, 10]. Furthermore, these hybrid materials are simple to mill, stain, characterize, and repair. PICN has properties similar to human enamel, but it cannot recover once it is unloaded [8, 11]. This material is more damage-resistant than regular ceramics because cracks are redirected at the polymer-ceramic interface, reducing the risk of chipping and failure [12]. SEM analysis confirms its strong stress-handling capabilities [13].
When it comes to cementing CAD/CAM milled restorations, there are different types of luting agents available. One such agent is the Glass Ionomer cement-based luting agent (GIC), which is a blend of dental silicate cement and zinc polycarboxylates. GIC is a versatile material that creates a chemical bond with tooth structure [14]. It's also biocompatible and bioactive with strong anti-caries properties, making it great for restorative dentistry [14, 15]. Clinicians commonly use GIC luting agents to attach zirconia crowns, as research shows that they remained strong when luted with this cement up to 0.5 mm thickness. GIC can also be used for luting of high-strength all-ceramic restorations like lithium disilicate glass-ceramic and oxide ceramic restorations and fixed partial dentures (FPD) if retention is sufficient [16]. Resin luting agents are low-viscosity composites used for various applications, such as the cementation of veneers, inlays, and orthodontic appliances. These materials are great for cementing ceramic and composite restorations, as well as cast restorations that need more retention [16]. They have a thin layer and good working and setting times. Resin luting agents are classified as self-cured, light-cured, or dual-cured. Dual-cured materials offer convenience and safety, with high conversion rates even in non-exposed areas. There are two types of materials: self-adhesive cements and those that need a separate adhesive for application [14, 16].
Choosing the correct abutment tooth and luting material is crucial for achieving a durably bonded CAD/CAM milled restoration [14, 16, 17]. Studies have indicated that the adhesion durability of a crown may be impacted by the type of luting agent used, but the detachment rate remains unaffected [14, 16, 18]. It is recommended to use resin cement for optimal outcomes, as its composition closely resembles that of hybrid ceramic crown materials [17, 19]. Glass-ceramic and zirconia crowns were found to be stronger when bonded with multistep resin composites than when conventionally cemented [18, 20]. A study by Indergård et al. found a significant increase in the fracture load of 3Y-zirconia crowns when using adhesive bonding instead of traditional zink phosphate luting agents [19]. Ceramic and composite anterior crowns had similar load-bearing capacity with GIC or self-adhesive resin luting agents, per a study by Stawarczyk et al. [21]. Whereas premolar full-coverage restoration’s load-bearing capacity was indeed affected by the type of luting agent, according to Masuda et al. [22]. In a recent finite element analysis (FEA), it was concluded that maxillary second molars are subjected to the highest occlusal stresses in centric occlusion [23]. Thus, the restoration of these teeth would necessitate the use of materials with a greater load-bearing capacity than those used for other teeth. As far as the authors know, there is currently no research available that can determine if the load-bearing capacity and fracture pattern of PICN hybrid ceramic CAD/CAM full-coverage single-tooth restorations for second maxillary molars are affected by the type of luting agent used. This study aimed to analyze the impact of two types of resin-based luting agents and one non-resin-based traditionally used luting agent on the load-bearing capacity of CAD/CAM milled PICN hybrid ceramic full-coverage single-tooth restorations. The null hypothesis was that there is no significant difference in the load at fracture between PICN hybrid ceramic crowns cemented with three different luting agents.
Materials and Methods
Study design
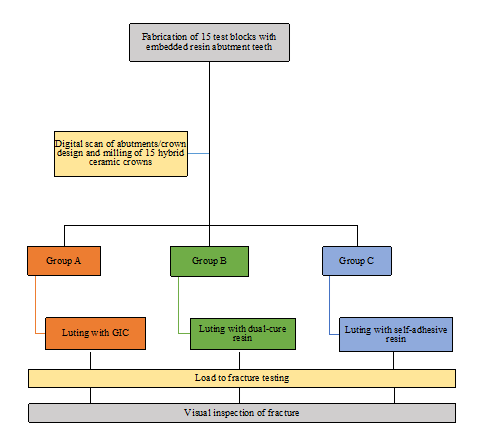
In this in-vitro study, a universal testing machine was used to measure the maximum load at fracture (load-bearing capacity) in three different groups based on the luting agent used. A total of 15 identical CAD/CAM crowns were milled from PICN hybrid ceramic blocks. Each crown had a contour thickness of 1.0 mm and a circular outer circumference to maintain a consistent axial thickness. The crowns were randomly divided into three groups (n=5) and placed on identical resin test blocks. Each group was cemented using one of three luting agents: GIC, self-adhesive dual-cure resin, and a dual-cure resin with a separate bonding agent. All cemented crowns were stored in distilled water at 37°C for 24 hours, then mounted in a universal testing machine and loaded till fracture. The maximum load at fracture for all crowns was recorded and statistically compared. Fractured restorations were inspected visually and compared descriptively between groups (Figure 1).
 |
|
Figure 1. Study design. |
Abutment teeth preparation
To create 15 abutment teeth, we duplicated a pre-prepared model acrylic maxillary second molar (UR72A, Nissin Dental Products Inc. in Kyoto, Japan). The tooth used as a master model abutment was adjusted according to specific criteria with an occlusal reduction of 1 mm. The height of the tooth crown was set at 5 mm for both buccal and lingual aspects, and 2.5 – 3 mm for the mesial and distal aspects. The crown width was confirmed to be 8 mm mesiodistally and 11 mm buccolingually. A uniform 1 mm circumferential heavy chamfer finish line was created, and the axial surface taper was set at 6 degrees. The occlusal form of the abutment teeth matched the natural tooth anatomy with rounded line angles.
A specially designed mold former was used to secure a duplicate of the model tooth. The silicone duplication material (Dublisil® 20 speed from Dreve Dentamid GmbH in Unna, Germany) was mixed and poured according to the manufacturer's instructions. The silicone was allowed to set for 30 minutes before carefully removing the model tooth. High-precision die resin (Mirapont, Hager & Werken GmbH & Co. KG, Duisburg, Germany) was used to make the duplicate abutment teeth. The mixture was prepared following the instructions provided by the manufacturer. It was mixed for 15 to 30 seconds until a smooth and even mixture was obtained. The mixture was then poured into a silicone mold in a thin line from a height of approximately 20 cm. A vibrating device (Whip Mix vibrator, Whip Mix Corporation, Louisville, KY, USA) was used at a very low vibration to ensure the mixture was evenly distributed. After 2 hours, the duplicate abutment tooth was removed from the mold (Figures 2a-2f).
The roots of the duplicated teeth were smoothed and standardized to 11.5-12 mm in length. They were then sandblasted with 110 µm Aluminum oxide particles. To simulate natural tooth mobility, the sand-blasted roots were coated with a thin layer of elastic latex material (ERKODENT Erkosin, Erich Kopp GmbH, Herrenberg, Germany), 1 mm away from the finish line [24, 25]. This resulted in a latex thickness of approximately 0.55 ± 0.1 mm apically, mimicking the resilience of natural periodontal tissue (Figures 2g-2i).
|
|
|
|
|
a) |
b) |
c) |
|
|
|
|
|
d) |
e) |
f) |
|
|
|
|
|
g) |
h) |
i) |
|
Figure 2. Duplication of the master model abutment tooth. A, b) The master model tooth secured within the mold former. c) mixing of duplication silicone. d) High-precision resin for abutment fabrication. e) Silicone mold with resin poured in. f) Resultant silicone mold and duplicate prepared abutment tooth. g) Duplicate resin teeth with rounded sandblasted roots. h) Erkodent liquid latex material. i) Duplicate resin teeth with a latex layer covering the root portions. |
||
Fabrication of the test blocks
The latex-covered roots of the duplicated teeth were embedded in high-precision resin (Mirapont, Hager & Werken GmbH & Co. KG, Duisburg, Germany) within cylindrical silicone molds (Dublisil® 20 speed, Dreve Dentamid GmbH, Unna, Germany) to fabricate the test blocks. The coronal portion and finish line were protected with wax beforehand till 3 mm apical to the finish line. After 2 hours, the test blocks were pulled out of the silicone molds. Statistical analysis was conducted using SPSS version 26 to get descriptive statistics as well (Figure 3a).
CAD/CAM fabrication of restorations
Scanning of the prepared teeth was done using Ceramill Map 400 Scanner (AmannGirrbach GmbH, Koblach, Austria). The design of the occlusal surface of the final restoration was completed using an adult molar design supplied by design software (Ceramill Mind, AmannGirrbach GmbH, Koblach, Austria). The complete crown design and dimensions were guided by the manufacturer's recommendation for Vita Enamic blocks (VITA Zahnfabrik H. Rauter GmbH & Co.KG, Bad Säckingen, Germany), with a circumferential axial thickness of 1 mm, and occlusal thickness of 1.5 mm measured in the central groove. The cement space was set at 20 μm in the region 1.0 mm above the margin and 60 μm in other regions (Figure 3b).
The hybrid ceramic crowns were milled to full anatomic contour from high translucency PICN Vita Enamic hybrid ceramic blocks shade 0M1 HT (VITA Zahnfabrik H. Rauter GmbH & Co.KG, Bad Säckingen, Germany) using the Ceramill Motion 2 machine (AmannGirrbach GmbH, Koblach, Austria) Wet milling was used with four diamond burs of varying sizes: 1.8 mm, 1.4 mm, 1.0 mm, and 0.4 mm. Then, the crowns were finished and polished according to the manufacturer’s instructions. All crowns were glazed with a light-cured characterization resin (GC Optigalze Color, GC Germany GmbH, Bad Homburg, Germany) (Figure 3c).
|
|
|
a) |
|
|
|
b) |
|
|
|
c) |
|
Figure 3. Resin test blocks: a) Resin test blocks with embedded duplicate abutment teeth. b) Digital scan and design of the tested PICN hybrid ceramic crown. c) Resin test blocks with cemented crowns. |
Cementation of the crowns
For this study, the test blocks were split into three groups (each with a sample size of 5) based on the type of luting agent used: Group A used GIC, Group B used dual-cured resin, and Group C used self-adhesive dual-cure resin. To prepare for the cementation procedure, the restorations were degreased with ethanol. The inner surfaces of the crowns were treated with 5% hydrofluoric acid gel (VITA Ceramics Etch, VITA Zahnfabrik H. Rauter GmbH & Co.KG, Bad Säckingen, Germany) for 60 seconds, while the outer surfaces were protected to prevent any unintended etching. Followed by silane application (Silane, Ultradent Products Inc, South Jordan, UT, USA) for 60 seconds, according to the manufacturer’s instructions. All test blocks were cleaned with ethanol to remove any debris before cementing the crowns.
Group A
A self-curing GIC luting agent (Vivaglass CEM, Ivoclar Vivadent AG, Schaan, Liechtenstein) was mixed according to the manufacturer’s instructions and applied to the inner surface of the milled crowns. The crowns were cemented on the prepared duplicate abutment with finger pressure until complete setting and the excess luting agent was cleaned from the margins.
Group B
The abutments were acid etched with 37% phosphoric acid (TotalEtch, Ivoclar Vivadent AG, Schaan, Liechtenstein) for 30 seconds, then rinsed with water and dried with air for 15 seconds. A universal bonding agent (Scotchbond Universal, 3M ESPE, ST. Paul, MN, USA) was applied to the abutments and the inner surfaces of the milled crowns and then cured for 20 seconds. A dual-cure resin luting agent (RelyX™ Ultimate Clicker, 3M ESPE, ST. Paul, MN, USA) was applied to the fitting surface of each crown then the crowns were then seated with finger pressure and tack light-cured for 2 seconds. Cement excesses were removed with a #12 scalpel, and the cement was allowed to fully cure for 6 minutes while maintaining finger pressure throughout.
Group C
A self-adhesive self-cure resin with tack light-cure option (Multilink Speed, Ivoclar Vivadent AG, Schaan, Liechtenstein) was applied to the fitting surface of the milled crowns then the crowns were seated with the same finger pressure, and tack cured for 2 seconds. The excess luting agent at the margins was removed with a #12 scalpel and finger pressure was maintained for 5 minutes to allow full polymerization of the luting agent.
Maximum load at fracture test and statistical analysis
The test blocks were kept in distilled water at a temperature of 37°C for 24 hours. Next, the test blocks were mounted on a universal testing machine (UTS) (5940 Series UTS (2 kN load cell), Instron, Norwood, MA, USA). To distribute the load on the occlusal surface, a 0.3 mm thick tin foil was placed between the rounded load and the crown. The position and contact of the 3.0 mm semi-cylindrical stainless-steel indenter of the UTS were verified for all samples before the commencement of the static fracture test. The load was applied along the long axis of the tooth. The test was conducted with a crosshead speed of 0.5 mm/minute until failure, which was set at a reduction in force of 10 Newtons (N).
The maximum load at fracture for each crown in every group was recorded, and descriptive statistics were calculated. The means of the maximum load at fracture (ML) for each group was calculated and then compared using a two-way ANOVA statistical test at a significance level of p<0.05. The fracture lines and cracks that resulted were inspected visually and compared between the groups.
Results and Discussion
The data analysis was conducted using the Statistical Program of Social Science version 18.0 (SPSS Inc, Chicago, USA). Descriptive statistics of the maximum loads at fracture (in Newtons (N)) for the PICN hybrid ceramic crowns that are luted with three different luting agents (Group A= GIC, Group B= dual-cure resin, and Group C= self-adhesive resin) are detailed in the following table (Table 1).
Table 1. Descriptive statistics for the maximum loads at fracture of the test groups.
|
|
n |
Max |
Min |
Median |
Mean |
SD |
|
Group A |
5 |
1036.45 |
762.99 |
907.61 |
896.27 |
122.26 |
|
Group B |
5 |
1141.26 |
768.88 |
936.04 |
959.13 |
148.39 |
|
Group C |
5 |
1322.7 |
814.43 |
1093.25 |
1030.46 |
213.07 |
Note. SD= standard deviation, Max= maximum value in Newtons, Min = minimum value in Newtons.
The mean maximum load at fracture of group C was the highest (1030.46 ± 213.07 N), followed by group B (959.13 ± 148.39 N), then group A (896.27 ± 122.26 N). Showing a higher load-bearing capacity of the hybrid ceramic crown when luted with self-adhesive resin cement (Figure 4).
|
|
|
Figure 4. The maximum loads at fracture values in Newtons for the cemented crowns in the three tested groups. |
The Kolmogorov-Smirnov Test of Normality was conducted and confirmed the normal distribution of the load at fracture values within the three groups (p>0.05). Levene test showed homogeneity of variances (p = 0.647) and therefore, one-way analysis of variance (ANOVA) was conducted to compare the groups at a significance level of 0.05. There was no statistically significant difference in the maximum load at fracture between the groups (Table 2).
Table 2. One-way analysis of variance (ANOVA) for the maximum loads at fracture of the test groups.
|
|
SS |
df |
MS |
F-ratio |
P |
|
Between groups |
45075.97 |
2 |
22537.99 |
0.8209 |
0.4633 |
|
Within groups |
329466.29 |
12 |
27455.52 |
||
|
Total |
374542.27 |
14 |
|
Note. SS = sum of squares, df = degrees of freedom, MS = mean of squares, P = Significance value (p>0.05, not significant).
Visual inspection of the fractured crowns revealed dislodged fracture fragments in response to the applied occlusal load. After conducting fracture tests on Group A, the crown fragments became detached from the abutments. In all groups, the main fracture line ran in a buccolingual direction through the central fossa in the occlusal surface, one group C and two group B test blocks had the main fracture line run through the mesial fossa instead. Test blocks in groups B and C showed fracture into two parts, with the smaller fragment chipping away while the rest of the crown remained bonded to the underlying resin abutment. It was noticed that the resin luting agents remained on both the abutment tooth surface and the inner surface of the crown. To assess the fracture pattern, the position of the main fracture line, the number of fractured fragments, and the detachment of the crown from the underlying abutment were used as reference points (Table 3).
Table 3. Visual inspection results of fracture pattern in the test groups.
|
|
Group A |
Group B |
Group C |
|
The mean number of fragments |
2.8 |
2 |
|
|
Main fracture line position |
Central fossa |
Central fossa, some mesial fossa (2 in each group) |
|
|
Fragments detachment |
All fragments |
Only smaller fragment |
|
Note. *= standard deviation, **= fracture through central fossa, ***= fracture through mesial fossa.
An increasing number of individuals are seeking dental restorations with enhanced esthetics, including those for their posterior teeth [22]. The present study tested full-coverage restorations milled using CAD/CAM technology from esthetic hybrid ceramic blocks. The study revealed variations in the maximum load at fracture between the groups. Nevertheless, no significant statistical differences were found between them. Thus, the null hypothesis stating that there was no significant difference in the maximum load at fracture among PICN hybrid ceramic crowns cemented with three different luting agents had to be accepted (p>0.05). All tested crowns in the current study had normal stress-strain curves, confirming the validity of the experimental design and ruling out any incorrect occlusal loading induced by the testing apparatus or test block material.
To minimize variability between the milled full-coverage restorations (crowns), PICN hybrid ceramic prefabricated CAD/CAM blocks (Vita Enamic, VITA Zahnfabrik H. Rauter GmbH & Co.KG, Bad Säckingen, Germany) were used to mill full-coverage crowns using the same design software (Ceramill Mind, AmannGirrbach GmbH, Koblach, Austria) and milling equipment (Ceramill Map 400 Scanner, AmannGirrbach GmbH, Koblach, Austria). For ceramic and hybrid ceramic materials, a minimum occlusal thickness of 1.5 mm is recommended for CAD/CAM milled crowns to withstand biting forces [22]. The CAD/CAM PICN hybrid ceramic crowns milled in the current study had a thickness of 1.5 mm at the central groove and 2.5 mm at the apex of the cusps. These dimensions are comparable to those suggested in Zimmerman et al.'s study, where a thickness of 1.5 mm was discovered to have the highest load at fracture values when compared to 0.8 and 0.5 mm [26]. To ensure accurate fitting of the milled crowns, each test block was scanned individually. This reduces the chances of any crown misfit affecting the resultant maximum load values. For crowns, it's important to make sure they match the other teeth and have the right cuspal inclination for bearing loads, since cuspal inclination was found, by Kuroishi et al., to significantly affect milled crowns' load-bearing capacity [27]. For this study, all crowns had the same occlusal anatomical design and cuspal inclinations - specifically, an adult, anatomic maxillary molar as supplied by the CAD software. This was done to simulate a clinical situation while ensuring the absence of differences between the tested restorations that could potentially affect the load results.
In previous studies, various techniques were used to ensure the correct placement of indirect restorations during cementation. These techniques included applying finger pressure, using a universal testing machine to control static loading, or not mentioning a specific method [25, 28]. To minimize the possibility of pressure variability, a single investigator seated all milled crowns in the current study. This was done because it was reported in the literature that finger pressure varies from person to person [25]. Prior studies cited in the literature have utilized this approach [25, 29]. The current study utilized finger pressure for seating, which could result in varying cement film thicknesses when compared to other studies that employ different methods. As a result, there may be potential discrepancies between the findings of this study and those of others.
Teeth in the oral cavity are subject to various forceful pressures during rest and mastication. These are absorbed by the periodontal ligament (PDL), which allows for a certain degree of movement of the teeth in the alveolar bone [30]. During an in-vitro load at fracture test, the tooth embedment material must emulate bone and supporting PDL to withstand masticatory forces and resist compression and other applied forces [31]. PDL simulation was found to have a greater impact on the fracture load test results than the embedment material type [32]. In the current study, liquid latex rubber (ERKODENT Erkosin, Erich Kopp GmbH, Herrenberg, Germany) was directly painted on the root portions of abutments embedded in the test blocks to simulate the PDL. This technique was found to be effective [33] and was utilized in multiple previous studies [24, 34]. In different in-vitro load-bearing capacity studies, several types of resins have been utilized for alveolar bone simulation in the test blocks [24, 25]. The elastic moduli of resins (around 2000 MPa) are closer to the alveolar bone than metal alloys, which have a much higher elastic modulus [35]. To mimic the natural bone support of teeth and ensure proper crown placement in this study, the abutment roots were set in isocyanate model resin test blocks (Mirapont, Hager & Werken GmbH & Co. KG, Duisburg, Germany) with flexural modulus closer to maxillary bone (around 14,000 MPa [36]) than that of stainless steel metal used in other load-bearing capacity studies (around 100,000 MPa [37]). [21, 22, 27] A 3 mm gap was left below the finish line so that the test block resin would not interfere with the abutment's finish line, abutment scan, and/or crown seating. This gap emulated the biological width [38] that should be maintained in clinical cases.
Previous studies indicated that the material of the abutment for restoration’s load-bearing capacity test could affect the maximum load at fracture values [22, 27, 31, 39, 40]. According to Sakaguchi et al., the use of metal abutments results in significantly lower fracture loads for crowns compared to those tested on resin abutment teeth [31]. Lan et al. concluded that using zirconia abutments resulted in higher loads at fracture for the tested crowns than softer abutment materials such as resins [40]. For this study, the abutment teeth and test blocks were made from a model resin material (Mirapont, Hager & Werken GmbH & Co. KG, Duisburg, Germany) with very low polymerization shrinkage (0.02%), like the model resin used in previous load-bearing studies [24, 41]. This would ensure the fabrication of accurate abutment teeth duplicates with very low variation between the duplicates. Resin materials were also found to have flexural properties closer to natural tooth structure than metallic materials [39, 41]. Thus, utilizing the high-precision, low-shrinkage resin for the fabrication of abutment teeth would ensure the easy, accurate, and standardized duplication of the model abutment tooth while mimicking the natural teeth structure. PICN hybrid ceramic CAD/CAM, containing a sintered-glass ceramic network that is 86% by weight and 75% by volume, has an elastic modulus of 30,000 MPa, which is also close to that of natural dentin [42].
CAD/CAM crowns can fail clinically due to detachment, but they can also fail due to fracture [43]. To test the load-bearing capacity in the present study, the load was applied axially perpendicular to the occlusal surface while using a 0.3 mm tinfoil to distribute the load on the occlusal surface. It was reported previously that the direction of the applied force on the restoration affects the resultant maximum load at fracture value [44]. The use of either tin foil or silicone rubber to distribute the load was utilized in previous studies testing the load-bearing capacity of indirect restorations [24, 41]. The grooves and fissures on the occlusal surface of teeth are areas where cracks can occur. The maxillary second molar experiences the highest amount of stress during centric closing and lateral excursive movements [22, 23]. Additionally, premolar crowns fractured along the central groove in a previous study by Masuda et al. [22]. In the current study, most main fracture lines occurred in the central fossa in a bucco-lingual direction fracturing the crown into two fragments, with only a few having the main fracture line going through the mesial fossa. The fracture of the crowns up with no chipping in the current study was observed in a previous study of ceramic and hybrid ceramic crowns by Güleç et al. [42]. In the GIC cemented crowns group the number of fractured fragments (mean 2.8 fragments) was more than those cemented with resin luting agents. A smaller fragment closer to the cervical third of the tooth that detached from the underlying abutment was observed in some of the group A samples. It could have been that a higher concentration of stress on the occlusal surface transmitted to the cervical thirds of the crowns in this group. This could be due to the non-adherent luting media having a reduced capability to distribute stress. The lower flexural and compressive strength and elastic modulus of GIC luting agents compared to dual-cure resin cement were reported in a previous study [45]. In previous studies, it was proposed that PICN hybrid ceramic CAD/CAM crowns may withstand compressive forces better than more brittle ceramic and zirconia materials [22, 27] and that the emergence of multiple fracture lines appears to signify the highest point of the fracture load of a CAD/CAM crown [22]. In this study, crowns from groups B and C showed occlusal compressive deformation, indicating that stresses were likely more evenly distributed and absorbed through the stronger resin luting agents and underlying resin abutment (all similar elastic moduli). These crowns were also bonded to the abutment and luting agent, which could have made them more resistant to loads than if they had been luted with a weaker agent like GIC. The larger fragment of the fractured crowns in groups B and C remained bonded to the underlying abutment, which could be advantageous in clinical situations by reducing the risk of large fragment aspiration by the patient. Additionally, retaining a portion of the crown that remains attached to the underlying tooth can reduce the negative aesthetic impact of a fractured crown.
Regarding the effect of the luting agent on the load-bearing capacity of PICN hybrid ceramic crowns in the current study, there was no statistically significant difference in the maximum load-at fracture between the different luting agent groups. This result is partly in accordance with a previous similar study by Masuda et al., which concluded the absence of a significant difference in load-bearing capacity of hybrid ceramic CAD/CAM crowns fixed on premolars (around 2800 N) using either traditional or self-bonding resins. However, the load was higher than those cemented with polycarboxylate luting agent [22]. On the other hand, Kuroishi et al. found no significant difference in load-bearing capacity between hybrid ceramic crowns cemented with resin or polycarboxylate [27], which could correlate with the absence of significant difference results of the current study. The higher loads in those studies compared to the current study (maximum 1322.7 N), might be attributed to their use of stronger hybrid ceramic material, different cement space and axial inclination, and the simpler occlusal anatomy of premolars compared to maxillary molars. However, the results of both studies suggest that CAD/CAM crowns may achieve greater fracture strength by resin bonding to the abutment teeth, which is in accordance with the results of a previous study on high-strength ceramic CAD/CAM crowns by Blatz et al. [18]. In the current study, crowns fixed with self-bonding luting resin had the highest maximum load at fracture (1030.46 ± 213.07 N), followed by dual-cure resin with a separate bonding agent (959.13 ± 148.39 N), then GIC (896.27 ± 122.26 N). This correlates with Kuroishi et al. study where self-bonding luting resins produced the highest loads at fracture but were statistically insignificant [27]. Sagoz et al. demonstrated that GIC luting cements produced lower loads at fracture in CAD/CAM premolar crowns compared to resin luting agents [46]. However, Stawarczyk et al. found no significant difference in the load-bearing capacity of resin anterior crowns cemented with either resin or GIC [21]. Self-bonding luting resins have low elastic moduli and thus can exhibit flexibility with high resistance to loads [27]. The mean maximum load at fracture of PICN hybrid ceramic crowns luted with self-bonding resin in the current study is similar to that found in previous studies by Zimmermann et al. (around 1063 N) [26] and Elmougi et al. (around 1127 N) [41].
Previous studies have shown that the total occlusal forces exerted on posterior teeth during closing and swallowing are around 100 N, ranging from 40 N for a light bite to 200 N for a hard bite [47]. The average clenching occlusal load is 660 N [48]. The mean maximum load at fracture of the crowns in all groups was well above the average occlusal load. Thus it can be concluded that PICN hybrid ceramic molar crowns are suitable for posterior teeth restoration, even with the presence of clenching. The difference in maximum load between the groups, even though not statistically significant, might be of clinical significance since the difference between the groups was higher than the light bite 40 N and closer to the lead of closing and swallowing. Maximum biting force might reach up to over 1000 Newtons in the posterior region of the mouth due to stress or parafunctional habits such as bruxism [49]. The mean maximum load at fracture of group C (self-bonding resin luting agent) was above 1000N, which suggests the advantageous effect of self-boning resin luting on PICN hybrid ceramic crowns in cases of bruxism and other parafunctional habits.
It should be noted that the current study only utilized a static load test and did not include mechanical fatiguing or thermal aging. However, as crown dislodgement is a prevalent cause of failure in full-coverage restorative clinical cases [27], it would be advantageous for future studies to incorporate dynamic load testing with chewing simulation to better reflect real-life scenarios. Therefore, this limitation should be addressed in future research. To evaluate the effectiveness of PICN hybrid ceramics in different scenarios, such as with varying opposing dentitions, crown thicknesses, and cement thicknesses, an in-vivo study could be carried out to examine their clinical performance. It should be noted that there are certain limitations in the study, particularly in regard to the impact of luting cement on the bond strength and marginal fit of various crown designs. The effects of occlusal anatomy and thickness, as well as the finishing and polishing procedures used on hybrid ceramic crowns, were also not fully examined. Additionally, the influence of axial thicknesses was not thoroughly explored. If a full-coverage crown treatment fails because of a fracture, it's a significant issue that should be addressed seriously. Employing Finite Element Analysis (FEA) could help recognize the areas of highest stress distribution in relation to the luting agent or cement space designed in CAD software.
Conclusion
Within the limitations of the study, it can be concluded that using self-bonding luting resin had a positive impact on the load-bearing capacity of PICN hybrid ceramic crowns specifically for molars. The impact of luting agent type on CAD/CAM crown fracture loads appears to be minimal. The CAD/CAM PICN hybrid ceramic is a great option for restoring posterior teeth, regardless of the type of cement used. This is because the maximum loads required to cause a fracture in the crowns were higher than the loads typically experienced by molars in clinical situations. As seen through visual inspection, GIC displayed more catastrophic fractures in the crowns than both resin-luting agents. However, evidence suggests that resin may be a more favorable option than GIC.
Acknowledgments: The authors would like to acknowledge with thanks The Advanced Technology Dental Research Laboratory (ATDRL), Faculty of Dentistry, King Abdulaziz University, for their technical support.
Conflict of interest: None
Financial support: None
Ethics statement: This in-vitro study was carried out after obtaining the ethical exemption from the research ethics committee of the Faculty of Dentistry at King Abdulaziz University (IRB protocol #08-12-19).
1. Prithviraj DR, Bhalla HK, Vashisht R, Sounderraj K, Prithvi S. Revolutionizing restorative dentistry: an overview. J Indian Prosthodont Soc. 2014;14(4):333-43.
2. Sulaiman TA. Materials in digital dentistry—A review. J Esthet Restor Dent. 2020;32(2):171-81.
3. Rekow ED. Digital dentistry: The new state of the art—Is it disruptive or destructive? Dent Mater. 2020;36(1):9-24.
4. Gwon B, Bae EB, Lee JJ, Cho WT, Bae HY, Choi JW, et al. Wear Characteristics of Dental Ceramic CAD/CAM Materials Opposing Various Dental Composite Resins. Materials. 2019;12(11):1839.
5. Alrakkad IA, Alrakkad RA, Altamimi MS, Alshammari NM, Alghuraymil AAS, John MAM, et al. Review on Dental Implant and Infection Management Approach. Arch Pharm Pract. 2022;13(1):37-9.
6. Yaghini J, Salmani SM, Hasheminejad SM, Mogharehabed A. Dentists’ Attention to Periodontal Therapy in the Patients Treatment Planning to Dental Clinics of Isfahan City. Arch Pharm Pract. 2022;13(2):51-6.
7. Lucena M, Relvas A, LefranÇOis M, Azevedo M, Sotelo P, Sotelo L. Resin matrix ceramics – mechanical, aesthetic and biological properties. RGO - Rev Gaúcha Odontol. 2021;69:e20210018.
8. Skorulska A, Piszko P, Rybak Z, Szymonowicz M, Dobrzyński M. Review on polymer, ceramic and composite materials for cad/cam indirect restorations in dentistry—Application, mechanical characteristics and comparison. Materials. 2021;14(7):1592.
9. Spitznagel F, Scholz K, Vach K, Gierthmuehlen P. Monolithic Polymer-Infiltrated Ceramic Network CAD/CAM Single Crowns: Three-Year Mid-Term Results of a Prospective Clinical Study. Int J Prosthodont. 2020;33(2):160-8.
10. Della Bona A, Corazza P, Zhang Y. Characterization of polymer-infiltrated ceramic-network material. Dent Mater. 2014;30(5):564-9.
11. Palacios T, Tarancón S, Pastor JY. On the Mechanical Properties of Hybrid Dental Materials for CAD/CAM Restorations. Polymers. 2022;14(16):3252.
12. El Zhawi H, Kaizer MR, Chughtai A, Moraes RR, Zhang Y. Polymer infiltrated ceramic network structures for resistance to fatigue fracture and wear. Dent Mater. 2016;32(11):1352-61.
13. Li W, Sun J. Effects of Ceramic Density and Sintering Temperature on the Mechanical Properties of a Novel Polymer-Infiltrated Ceramic-Network Zirconia Dental Restorative (Filling) Material. Med Sci Monit. 2018;24:3068-76.
14. Turkistani A, Islam S, Shimada Y, Tagami J, Sadr A. Dental cements: Bioactivity, bond strength and demineralization progression around restorations. Am J Dent. 2018;31(Sp Is B):24B-31B.
15. Yeslam HE, Hasanain FA. Evaluation of the Strength of a Novel Bioactive Hybrid Glass Restorative Material. J Biochem Technol. 2023;14(2):61-5.
16. Heboyan A, Vardanyan A, Karobari MI, Marya A, Avagyan T, Tebyaniyan H, et al. Dental Luting Cements: An Updated Comprehensive Review. Molecules. 2023;28(4):1619.
17. Calheiros-Lobo MJ, Vieira T, Carbas R, da Silva LFM, Pinho T. Effectiveness of Self-Adhesive Resin Luting Cement in CAD-CAM Blocks—A Systematic Review and Meta-Analysis. Materials. 2023;16(8):2996.
18. Blatz MB, Vonderheide M, Conejo J. The Effect of Resin Bonding on Long-Term Success of High-Strength Ceramics. J Dent Res. 2018;97(2):132-9.
19. Indergård JA, Skjold A, Schriwer C, Øilo M. Effect of cementation techniques on fracture load of monolithic zirconia crowns. Biomater Investig Dent. 2021;8(1):160-9.
20. Lawson NC, Jurado CA, Huang CT, Morris GP, Burgess JO, Liu PR, et al. Effect of Surface Treatment and Cement on Fracture Load of Traditional Zirconia (3Y), Translucent Zirconia (5Y), and Lithium Disilicate Crowns. J Prosthodont. 2019;28(6):659-65.
21. Stawarczyk B, Beuer F, Ender A, Roos M, Edelhoff D, Wimmer T. Influence of cementation and cement type on the fracture load testing methodology of anterior crowns made of different materials. Dent Mater J. 2013;32(6):888-95.
22. Masuda T, Nomoto S, Sato T, Kanda Y, Sakai T, Tsuyuki Y. Effect of Differences in Axial Thickness and Type of Cement on Fracture Resistance in Composite Resin CAD/CAM Crowns. Bull Tokyo Dent Coll. 2019;60(1):17-27.
23. Duanmu Z, Liu L, Deng Q, Ren Y, Wang M. Development of a biomechanical model for dynamic occlusal stress analysis. Int J Oral Sci. 2021;13(1):29.
24. Greuling A, Matthies A, Eisenburger M. Fracture load of 4-unit interim fixed partial dentures using 3D-printed and traditionally manufactured materials. J Prosthet Dent. 2023;129(4):607.
25. Alzahrani SJ, Hajjaj MS, Yeslam HE, Marghalani TY. Fracture Resistance Evaluation and Failure Modes Rating Agreement for Two Endocrown Designs: An In Vitro Study. Appl Sci. 2023;13(5):3001.
26. Zimmermann M, Egli G, Zaruba M, Mehl A. Influence of material thickness on fractural strength of CAD/CAM fabricated ceramic crowns. Dent Mater J. 2017;36(6):778-83.
27. Kuroishi G, Yotsuya M, Nomoto S, Hisanaga R, Sato T. Effects of Cuspal Inclination and Luting Agent on Fracture Load Values in Composite Resin CAD/CAM Crowns. Bull Tokyo Dent Coll. 2022;63(2):55-66.
28. Pedrollo Lise D, Van Ende A, De Munck J, Umeda Suzuki TY, Cardoso Vieira LC, Van Meerbeek B. Biomechanical behavior of endodontically treated premolars using different preparation designs and CAD/CAM materials. J Dent. 2017;59:54-61.
29. Kongkiatkamon S, Booranasophone K, Tongtaksin A, Kiatthanakorn V, Rokaya D. Comparison of Fracture Load of the Four Translucent Zirconia Crowns. Molecules. 2021;26(17):5308.
30. Reddy RT, Vandana KL. Effect of hyperfunctional occlusal loads on periodontium: A three-dimensional finite element analysis. J Indian Soc Periodontol. 2018;22(5):395-400.
31. Sakoguchi K, Minami H, Suzuki S, Tanaka T. Evaluation of fracture resistance of indirect composite resin crowns by cyclic impact test: influence of crown and abutment materials. Dent Mater J. 2013;32(3):433-40.
32. Sterzenbach G, Kalberlah S, Beuer F, Frankenberger R, Naumann M. In-vitro simulation of tooth mobility for static and dynamic load tests: a pilot study. Acta Odontol Scand. 2011;69(5):316-8.
33. Al zahrani F, Richards L. Micro-CT evaluation of a novel periodontal ligament simulation technique for dental experimental models. Arch Orofac Sci. 2018;13(2).
34. Sarafidou K, Stiesch M, Dittmer MP, Jorn D, Borchers L, Kohorst P. Load-bearing capacity of artificially aged zirconia fixed dental prostheses with heterogeneous abutment supports. Clin Oral Investig. 2012;16(3):961-8.
35. Scherrer SS, de Rijk WG. The fracture resistance of all-ceramic crowns on supporting structures with different elastic moduli. Int J Prosthodont. 1993;6(5):462-7.
36. Sozkes S. Dental Implant for Maxillary Cancellous Alveolar Bone with Expandable Transformation in Apical Part. Niger J Clin Pract. 2021;24(8):1126-32.
37. Alhassan EA, Olasehinde D, Musonda A, Odeniyi O. Tensile and flexural behaviour of steel materials used in the construction of crop processing machines. IOP Conf Ser: Earth Environ Sci. 2020;445(1):012044.
38. Aksel H, Askerbeyli S, Sungur D. Vertical root fracture resistance of simulated immature permanent teeth filled with MTA using different vehicles. J Clin Exp Dent. 2017;9(2):e178.
39. Bencun M, Ender A, Wiedemeier DB, Mehl A. Fracture Load of CAD/CAM Feldspathic Crowns Influenced by Abutment Material. Materials (Basel). 2020;13(15):3407.
40. Lan TH, Chen PH, Fok ASL, Chen YF. Contact fracture test of monolithic hybrid ceramics on different substrates for bruxism. Dent Mater. 2022;38(1):44-56.
41. Elmougy A, Schiemann AM, Wood D, Pollington S, Martin N. Characterisation of machinable structural polymers in restorative dentistry. Dent Mater. 2018;34(10):1509-17.
42. Güleç C, Sarıkaya I. The influence of aging on the fracture load of milled monolithic crowns. BMC Oral Health. 2022;22(1):516.
43. Miura S, Fujisawa M. Current status and perspective of CAD/CAM-produced resin composite crowns: a review of clinical effectiveness. Jpn Dent Sci Rev. 2020;56(1):184-9.
44. Seydler B, Rues S, Muller D, Schmitter M. In vitro fracture load of monolithic lithium disilicate ceramic molar crowns with different wall thicknesses. Clin Oral Investig. 2014;18(4):1165-71.
45. Dewan S, Tarun K, Kumar M, Bansal A, Avasthi A. Comparative Evaluation of Flexural Strength and Modulus of Elasticity of Three Adhesive Luting Cements at Different Time Intervals under Oral Simulated Conditions: An In Vitro Study. Dent J Adv Stud. 2021;9(02):70-6.
46. Sagsoz NP, Yanıkoglu N. Evaluation of the fracture resistance of computer-aided design/computer-aided manufacturing monolithic crowns prepared in different cement thicknesses. Niger J Clin Pract. 2018;21(4):417-22.
47. Kayumi S, Takayama Y, Yokoyama A, Ueda N. Effect of bite force in occlusal adjustment of dental implants on the distribution of occlusal pressure: comparison among three bite forces in occlusal adjustment. Int J Implant Dent. 2015;1(1):14.
48. Widmalm S, Ericsson S. Maximal bite force with centric and eccentric load. J Oral Rehabil. 1982;9(5):445-50.
49. Jansen van Vuuren L, Broadbent JM, Duncan WJ, Waddell JN. Maximum voluntary bite force, occlusal contact points and associated stresses on posterior teeth. J Roy Soc New Zeal. 2020;50(1):132-43.